Laboratories
- Back
- Top > Laboratories > Surgery > Pediatric Surgery
SurgeryPediatric Surgery
Introduction
A. Facility specializing in pediatric endoscopic surgery
Although the number of patients requiring pediatric surgery is small, their diseases markedly vary. Therefore, in order to appropriately treat such patients, it is important to intensively perform a large number of surgeries for them in a single facility. We perform more than 700 surgeries annually in- and outside the hospital, and are expected to play a central role in developing new treatment methods and educating/training pediatric surgeons as a high-volume center. We treat patients from the Tokai and other distant districts through collaboration with related departments (such as the Departments of Pediatrics, Obstetrics and Gynecology, Cardiovascular Surgery, Urology, Orthopedics, Ophthalmology, Otolaryngology, Plastic and Reconstructive Surgery, Anesthesiology, Intensive Care, and Internal Medicine). With Doctor Uchida, who has the most extensive experience of pediatric endoscopic surgery in Japan, assigned in August 2013 we treat patients with congenital esophageal atresia, congenital lung diseases, biliary atresia, congenital biliary dilatation, and other disorders requiring high-level endoscopic surgery, while considering appropriate methods to reduce the burden on these children daily.
B. Extensive experience of dealing with hepato-biliary-pancreatic diseases
Up to the present, we have actively dealt with hepato-biliary-pancreatic diseases, such as biliary atresia, congenital biliary dilatation, and liver transplantation. We perform treatment, while not only improving surgical treatment methods, but also examining countermeasures against complications and the challenges of long-term follow-up. As part of such treatment, we are also engaged in living donor liver transplantation to be performed within the hospital through collaboration with the Department of Transplantation Surgery.
C. Comprising the General Perinatal Medical Center to treat newborns requiring surgery
Our facility was designated as a General Perinatal Medical Center in Aichi Prefecture in April 2012. Such centers are medical institutions designated by municipalities to provide advanced medical services for pregnant females and newborns with severe conditions. The center consists of 2 major divisions: reproductive medicine/perinatal; and neonatal. The latter comprises the NICU and GCU with 12 and 24 beds, respectively, in addition to the Departments of Obstetrics, Pediatrics, and Pediatric Surgery which closely collaborate and regularly hold joint conferences. It provides surgical treatment for extremely-low-birth-weight infants and pediatric patients with congenital diseases requiring advanced management through collaboration with related departments and external medical institutions in the vicinity.
D. Designated as a pediatric cancer hub hospital
As a large number of hospitals deal with pediatric cancer despite the small number of patients with it, it is difficult for some hospitals to obtain extensive treatment experience in this area. As a solution, the Ministry of Health, Labour, and Welfare designated a pediatric cancer hub hospital to centralize patients with pediatric cancer refractory to treatment and those requiring highly specialized treatment, and provide them with high-quality medical services in each district. Such hospitals are selected based on the results of evaluation by experts from comprehensive perspectives, covering medical service systems/equipment, training systems, and clinical research activities, as well as treatment outcomes. Having been evaluated the most favorably nationwide, our department was selected as a hub hospital for the Tokai/Hokuriku/Shinetsu Block in February 2013, together with Mie University Hospital. In line with this, Nagoya University Hospital aims to establish more appropriate medical service systems by further improving the quality of staff and equipment for pediatric cancer treatment and cooperating with other medical institutions within the block.
Research Projects
We are engaged in basic and clinical research on various diseases, represented by the following studies:
Present research
Project title 1:
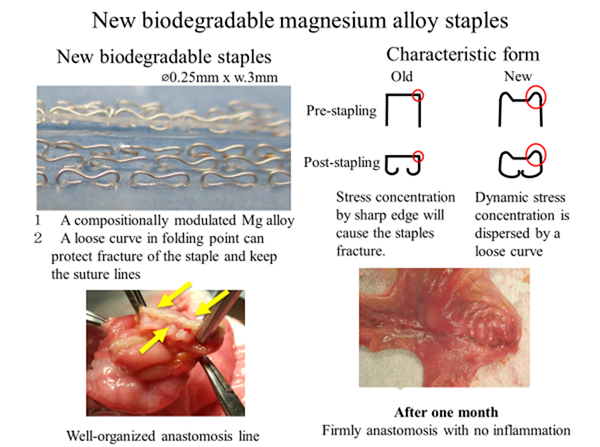
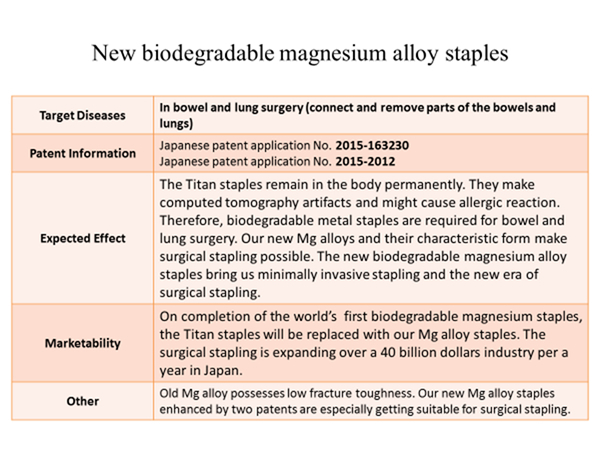
Development of a new biodegradable magnesium alloy ataples for bowel and lung surgery
Project title 2:
Development of a next generation photothermal therapy using a light-absorbing drug that selectively accumulates in lesions for pediatric cancer
ICG lactosome, a novel drug delivery system (DDS) type photothermal agent that is composed of polymeric micelle and indocyanine green (ICG), show a selective accumulation in cancer based on EPR effect. We showed the selective accumulation in tumors through animal experiments using the ICG lactosome and showed the utility in tumor imaging with the fluorescence derived from ICG as an indicator. On the other hand, ICG is known to be an infrared absorbing substance, thereby when a tumor in which ICG accumulate is irradiated with infrared light, only the tumor can be heated by photothermal reaction. We have found that when irradiation is performed so that the tumor temperature is 43 ° C or higher by adjusting the light output, the tumor can be eliminated with a probability of almost 100%.
Therefore, in this study, we aim to develop an endoscope based high efficiency cancer therapy system using ICG lactosome and a thermal control mechanism in order to treat the tumor lesions that can be reached with an endoscopic approach. When this therapeutic system becomes to be clinically applied, more selective diagnosis for tumor locations can be achieved for infiltrative tumors and metastatic tumors of childhood cancers than fluorescence imaging method using conventional ICG (without DDS). Moreover, curative treatment for the tumors by the photothermal reaction can be carried out simultaneously. This diagnostic and therapeutic system is minimally invasive and it is an innovative methodology that can be repeatedly applied until tumors disappear every time invasive lesions or metastatic lesions are found.
In the first half of the research period, ICG lactosome is administered to tumor model animals transplanted with childhood cancer cell lines (neuroblastoma / hepatoblastoma) transfected with a luminescent gene that express a high luminance, followed by photothermal treatment, suitable conditions (irradiation intensity and time, concentration of ICG lactosome, etc.) for maximizing the antitumor effects are to be elucidated especially for pediatric invasive or metastatic tumor. On the other hand, in order to realize the endoscope-based high-efficiency cancer treatment system with the photothermal control mechanism, we intend to fabricate three elemental technologies as follows; (i) an irradiation system that can efficiently deliver light to lesion sites, (ii) a thermography endoscope, (iii) a control system for tumor temperature. In the latter half of the period, animal models of orthotopic tumors are subjected to an endoscopic surgery with the developed integrated system in order to sublimate it into a technology that contributes to clinical use.
Keywords:
1 (pediatric cancer) 2 (neuroblastoma) 3 (hepatoblastoma) 4 (drug delivery system) 5 (ICG lactosome) 6 (photothermal therapy) 7 (tumor temperature) 8(invasive tumor)9(metastatic tumor)
Project title 3:
Determination of new biomarkers for pediatric cancer based on comprehensive analysis of urine metabolites
Pediatric cancer is a number-one cause of child mortality, but pediatric cancer control measures are still inadequate. In many cases, tumors have already metastasized to other organs and moved to other parts of the body when they are discovered, making treatment very difficult. A minimally invasive technique for early discovery of pediatric cancer could be expected to improve treatment success. In fact, for most cases the earlier pediatric cancer is treated, the better chance of success—early detection is directly related to prognosis. When it is difficult to remove tumors surgically or there is a chance that tumor mass remains even after surgery, chemo- or radiation therapy is often used, but when effective markers for tumors cannot be found, medical imaging can be the only effective diagnostic method. This applies to tumors such as Wilms’ tumors, striated muscle sarcoma, osteosarcoma, and the Ewing family of tumors. CT and PET imaging is effective in diagnosing remaining tumor, but when even these methods are not conclusive, very invasive treatments are needed to biopsy or remove remaining tumor mass. Even when techniques such as PET are conclusive in finding remaining tumor, it is used repeatedly over long periods in most pediatric cancer cases, raising considerable concern that the treatments themselves could be carcinogenic. For such tumors, discovery of non-invasive tumor markers would bring immeasurable benefit in diagnosis and treatment for children in the future. Metabolites in urine are stable and less affected by enzymes than substances in blood, so they hold promise as tumor markers. Urine tests are also easy to administer to children, so they can be used easily for screening. As such, we began a search of for new tumor markers in urine through a comprehensive analysis of urine metabolites. We are looking for tumor markers that are more sensitive and reflect more on the prognosis, even for
diseases for which markers are known already. The aims of our research are (1) early discovery of pediatric cancer through simple, non-invasive urine testing, and (2) to search for new markers in urine that will contribute to early detection of treatment effectiveness and recurrences for pediatric cancers that cannot be detected through blood sample tumor markers. Practically speaking, we will seek metabolites with potential as tumor markers by collecting urine samples from children, and performing a comprehensive analysis of urine metabolites using liquid chromatograph mass spectrometer.
Keywords:
1 (pediatric cancer) 2 (urine metabolite) 3 (liquid chromatograph mass spectrometer) 4 (Wilms’ tumor) 5 (striated muscle sarcoma) 6 (osteosarcoma) 7 (the Ewing family of tumor)
Past research
- Integrative studies on the pathology and treatment of pancreaticobiliary maljunction
- Studies on the pathogenesis of congenital biliary dilatation, focusing on the nervous system and function of the biliary tract
- Studies on cholangiocyte transplantation as a new treatment method for biliary atresia
- Studies on the mechanisms of extrinsic nerve growth in Hirschsprung’s disease
- Studies on biochemical/histological changes in the liver and hepatic metabolism during in vivo isolated hepatic perfusion
- Clinical studies on ECMO using pediatric blood pumps
Faculty Members
| Faculty | Position | Department |
|---|---|---|
| UCHIDA Hiroo | Professor | Pediatric Surgery, Children's Cancer Center |
| HINOKI Akinari | Designated Professor | Pediatric Surgery, Rare/Intractable Cancer Analysis Research |
| SHIROTA Chiyoe | Assistant Professor | Pediatric Surgery |
| SUMIDA Wataru | Lecturer of hospital | Pediatric Surgery, Children's Cancer Center |
| YOKOTA Kazuki | Assistant Professor of hospital | Pediatric Surgery |
| MAKITA Satoshi | Assistant Professor of hospital | Pediatric Surgery |
| OKAMOTO Masamune | Assistant Professor of hospital | Pediatric Surgery |
| TAKIMOTO Aitaro | Clinical fellow | Pediatric Surgery |
| YASUI Akihiro | Clinical fellow | Pediatric Surgery |
| TAKADA Shunya | Clinical fellow | Pediatric Surgery |
| NAKAGAWA Yoichi | Clinical fellow | Pediatric Surgery |
| AMANO Hizuru | Clinical fellow | Pediatric Surgery |
| KATO Daiki | Resident | Pediatric Surgery |
Bibliography
- 2021
- Yokoyama S, Ishizu Y, Ishigami M, Honda T, Kuzuya T, Ito T, Hinoki A, Sumida W, Shirota C, Tainaka T, Makita S, Yokota K, Uchida H, Fujishiro M: Factors associated with bleeding after endoscopic variceal ligation for children. Pediatr Int, 2021
- Yokota K, Uchida H, Sakairi M, Abe M, Tanaka Y, Tainaka T, Shirota C, Sumida W, Oshima K, Makita S, Amano H, Hinoki A: Identification of novel neuroblastoma biomarkers in urine samples. Sci Rep 11:4055, 2021
- Yamaguchi S, Hinoki A, Tsubouchi K, Amano H, Tajima A, Uchida H: Usefulness of web search queries for early detection of diseases in infants. Nagoya J Med Sci 83:107-111, 2021
- Tanaka Y, Tainaka T, Hinoki A, Shirota C, Sumida W, Yokota K, Oshima K, Makita S, Amano H, Takimoto A, Kano Y, Uchida H: Risk factors and outcomes of bile leak after laparoscopic surgery for congenital biliary dilatation. Pediatr Surg Int 37:235-240, 2021
- Takimoto A, Sumida W, Amano H, Shirota C, Tainaka T, Yokota K, Makita S, Yasui A, Kanou Y, Hinoki A, Uchida H: Postoperative intestinal obstruction in patients with biliary atresia impedes biliary excretion and results in subsequent liver transplantation. Pediatr Surg Int 37:229-234, 2021
- Takeda M, Sakamoto S, Uchida H, Shimizu S, Yanagi Y, Fukuda A, Uchida H, Yamataka A, Kasahara M: Comparative study of open and laparoscopic Kasai portoenterostomy in children undergoing living donor liver transplantation for biliary atresia. Pediatr Surg Int, 2021
- Shirota C, Tainaka T, Sumida W, Yokota K, Makita S, Takimoto A, Amano H, Hinoki A, Ono Y, Uchida H: Thoracoscopic surgery for congenital lung cysts: an attempt to limit pulmonary resection in cases of lesions involving multiple lobes. Pediatr Surg Int 37:213-221, 2021
- Shirota C, Kawashima H, Tainaka T, Sumida W, Yokota K, Makita S, Amano H, Takimoto A, Hinoki A, Uchida H: Double-balloon endoscopic retrograde cholangiography can make a reliable diagnosis and good prognosis for postoperative complications of congenital biliary dilatation. Sci Rep 11:11052, 2021
- Konishi KI, Mizuochi T, Takei H, Yasuda R, Sakaguchi H, Ishihara J, Takaki Y, Kinoshita M, Hashizume N, Fukahori S, Shoji H, Miyano G, Yoshimaru K, Matsuura T, Sanada Y, Tainaka T, Uchida H, Kubo Y, Tanaka H, Sasaki H, Murai T, Fujishiro J, Yamashita Y, Nio M, Nittono H, Kimura A: A Japanese prospective multicenter study of urinary oxysterols in biliary atresia. Sci Rep 11:4986, 2021
- Kawano T, Souzaki R, Sumida W, Shimojima N, Hishiki T, Kinoshita Y, Uchida H, Tajiri T, Yoneda A, Oue T, Kuroda T, Hirobe S, Koshinaga T, Hiyama E, Nio M, Inomata Y, Taguchi T, Ieiri S: Current thoracoscopic approach for mediastinal neuroblastoma in Japan-results from nationwide multicenter survey. Pediatr Surg Int, 2021
- Kawano T, Souzaki R, Sumida W, Ishimaru T, Fujishiro J, Hishiki T, Kinoshita Y, Kawashima H, Uchida H, Tajiri T, Yoneda A, Oue T, Kuroda T, Koshinaga T, Hiyama E, Nio M, Inomata Y, Taguchi T, Ieiri S: Laparoscopic approach for abdominal neuroblastoma in Japan: results from nationwide multicenter survey. Surg Endosc, 2021
- Amano H, Shirota C, Tainaka T, Sumida W, Yokota K, Makita S, Takimoto A, Tanaka Y, Hinoki A, Kawashima H, Uchida H: Late postoperative complications of congenital biliary dilatation in pediatric patients: a single-center experience of managing complications for over 20 years. Surg Today, 2021
- 2020
- Tanaka T, Amano H, Tanaka Y, Takahashi Y, Tajiri T, Tainaka T, Shirota C, Sumida W, Yokota K, Makita S, Tani Y, Hinoki A, Uchida H: Safe diagnostic management of malignant mediastinal tumors in the presence of respiratory distress: a 10-year experience. BMC Pediatr 20:292, 2020
- Shirota C, Murase N, Tanaka Y, Ogura Y, Nakatochi M, Kamei H, Kurata N, Hinoki A, Tainaka T, Sumida W, Yokota K, Makita S, Oshima K, Uchida H: Laparoscopic Kasai portoenterostomy is advantageous over open Kasai portoenterostomy in subsequent liver transplantation. Surg Endosc 34:3375-3381, 2020
- Sassa N, Yokoyama Y, Nishida Y, Yamada S, Uchida H, Kajiyama H, Nagino M, Kodera Y, Gotoh M: Clinical characteristics and surgical outcomes of retroperitoneal tumors: a comprehensive data collection from multiple departments. Int J Clin Oncol 25:929-936, 2020
- Ito Y, Asato K, Cho I, Sakai Y, Iwano K, Tainaka T, Uchida H: Intestinal flow after anastomotic operations in neonates. Comput Biol Med 118:103471, 2020
- Ishimaru T, Kawashima H, Tainaka T, Suzuki K, Takami S, Kakihara T, Katoh R, Aoyama T, Uchida H, Iwanaka T: Laparoscopically Assisted Anorectoplasty for Intermediate-Type Imperforate Anus: Comparison of Surgical Outcomes with the Sacroperineal Approach. J Laparoendosc Adv Surg Tech A 30:350-354, 2020
- Amano H, Miyake K, Hinoki A, Yokota K, Kinoshita F, Nakazawa A, Tanaka Y, Seto Y, Uchida H: Novel zinc alloys for biodegradable surgical staples. World J Clin Cases 8:504-516, 2020
- 2019
- Yokoyama S, Ishigami M, Honda T, Kuzuya T, Ishizu Y, Ito T, Hirooka Y, Tanaka Y, Tainaka T, Shirota C, Chiba K, Uchida H, Fujishiro M: Spleen stiffness by 2D shear wave elastography is the most accurate predictor of high-risk esophagogastric varices in children with biliary atresia. Hepatol Res, 2019
- Tanaka Y, Shirota C, Tainaka T, Sumida W, Oshima K, Makita S, Tanaka T, Tani Y, Chiba K, Uchida H: Efficacy of and prognosis after steroid pulse therapy in patients with poor reduction of jaundice after laparoscopic Kasai portoenterostomy. Pediatr Surg Int 35:1059-1063, 2019
- Takeshita T, Yoshida M, Takei Y, Ouchi A, Hinoki A, Uchida H, Kobayashi T: Relationship between Contact Pressure and Motion Artifacts in ECG Measurement with Electrostatic Flocked Electrodes Fabricated on Textile. Sci Rep 9:5897, 2019
- Takanari K, Toriyama K, Kambe M, Nakamura Y, Uchibori T, Ebisawa K, Shirota C, Tainaka T, Uchida H, Kamei Y: Nuss procedure for patients with pectus excavatum with a history of intrathoracic surgery. J Plast Reconstr Aesthet Surg 72:1025-1029, 2019
- Shirota C, Tanaka Y, Tainaka T, Sumida W, Yokota K, Makita S, Oshima K, Tanaka T, Tani Y, Uchida H: Therapeutic strategy for thoracoscopic repair of esophageal atresia and its outcome. Pediatr Surg Int 35:1071-1076, 2019
- Murase N, Tainaka T, Uchida H, Hinoki A, Shirota C, Yokota K, Oshima K, Shirotsuki R, Chiba K, Tanaka Y: A Novel Laparoscopic Surgery Model with a Device to Expand the Abdominal Working Space in Rats: The Influence of Pneumoperitoneum and Skin Incision Length on Postoperative Inflammatory Cytokines. J Invest Surg 32:55-60, 2019
- Murase N, Hinoki A, Shirota C, Tomita H, Shimojima N, Sasaki H, Nio M, Tahara K, Kanamori Y, Shinkai M, Yamamoto H, Sugawara Y, Hibi T, Ishimaru T, Kawashima H, Koga H, Yamataka A, Uchida H: Multicenter, retrospective, comparative study of laparoscopic and open Kasai portoenterostomy in children with biliary atresia from Japanese high-volume centers. J Hepatobiliary Pancreat Sci 26:43-50, 2019
- Amano H, Hanada K, Hinoki A, Tainaka T, Shirota C, Sumida W, Yokota K, Murase N, Oshima K, Chiba K, Tanaka Y, Uchida H: Biodegradable Surgical Staple Composed of Magnesium Alloy. Sci Rep 9:14671, 2019
- 2018
- Yokota K, Uchida H, Tainaka T, Tanaka Y, Shirota C, Hinoki A, Kato T, Sumida W, Oshima K, Chiba K, Ishimaru T, Kawashima H: Single-stage laparoscopic transanal pull-through modified Swenson procedure without leaving a muscular cuff for short- and long-type Hirschsprung disease: a comparative study. Pediatr Surg Int 34:1105-1110, 2018
- Togawa T, Mizuochi T, Sugiura T, Kusano H, Tanikawa K, Sasaki T, Ichinose F, Kagimoto S, Tainaka T, Uchida H, Saitoh S: Clinical, Pathologic, and Genetic Features of Neonatal Dubin-Johnson Syndrome: A Multicenter Study in Japan. J Pediatr, 2018
- Tanaka Y, Tainaka T, Uchida H: Indications for total esophagogastric dissociation in children with gastroesophageal reflux disease. Surg Today, 2018
- Tanaka Y, Tainaka T, Sumida W, Hinoki A, Shirota C, Murase N, Oshima K, Shirotsuki R, Chiba K, Uchida H: Introduction of resection of intrahepatic bile duct stenosis-causing membrane or septum into laparoscopic choledochal cyst excision. Pediatr Surg Int 34:1087-1092, 2018
- Takazawa S, Ishimaru T, Harada K, Deie K, Hinoki A, Uchida H, Sugita N, Mitsuishi M, Iwanaka T, Fujishiro J: Evaluation of Surgical Devices Using an Artificial Pediatric Thoracic Model: A Comparison Between Robot-Assisted Thoracoscopic Suturing Versus Conventional Video-Assisted Thoracoscopic Suturing. J Laparoendosc Adv Surg Tech A, 2018
- Tainaka T, Uchida H, Tanaka Y, Hinoki A, Shirota C, Sumida W, Yokota K, Makita S, Oshima K, Chiba K, Ishimaru T, Kawashima H: Long-term outcomes and complications after laparoscopic-assisted anorectoplasty vs. posterior sagittal anorectoplasty for high- and intermediate-type anorectal malformation. Pediatr Surg Int 34:1111-1115, 2018
- Sumida W, Uchida H, Tainaka T, Shirota C, Hinoki A, Kato T, Yokota K, Oshima K, Shirotuki R, Chiba K, Tanaka Y: Oral administration of eicosapentaenoic acid suppresses liver fibrosis in postoperative patients with biliary atresia. Pediatr Surg Int 34:1059-1063, 2018
- Sumida W, Uchida H, Ono Y, Tanaka Y, Tainaka T, Shirota C, Yokota K, Oshima K, Chiba
- 2017
- Murase N, Tainaka T, Uchida H, Hinoki A, Shirota C, Yokota K, Oshima K, Shirotsuki R, Chiba K, Tanaka Y. A Novel Laparoscopic Surgery Model with a Device to Expand the Abdominal Working Space in Rats: The Influence of Pneumoperitoneum and Skin Incision Length on Postoperative Inflammatory Cytokines. J Invest Surg. 2019 Jan;32(1):55-60.
- Amano H, Uchida H, Tanaka Y, Tainaka T, Mori M, Oguma E, Kishimoto H, Kawashima H, Arakawa Y, Hanada R, Koh K. Excellent prognosis of patients with intermediate-risk neuroblastoma and residual tumor postchemotherapy. J Pediatr Surg. 2018 Sep;53(9):1761-1765.
- Tanaka Y, Tainaka T, Sumida W, Shirota C, Hinoki A, Murase N, Oshima K, Shirotsuki R, Chiba K, Uchida H. The efficacy of resection of intrahepatic bile duct stenosis-causing membrane or septum for preventing hepatolithiasis after choledochal cyst excision. J Pediatr Surg. 2017 Dec;52(12):1930-1933.
- Amano H, Tanaka Y, Kawashima H, Deie K, Fujiogi M, Suzuki K, Morita K, Iwanaka T, Uchida H. Comparison of single-incision laparoscopic percutaneous extraperitoneal closure (SILPEC) and open repair for pediatric inguinal hernia: a single-center retrospective cohort study of 2028 cases. Surg Endosc. 2017 Dec;31(12):4988-4995.
- Amano H, Fujishiro J, Hinoki A, Uchida H. Intralobar pulmonary sequestration expanding toward the contralateral thorax: two case reports. BMC Surg. 2017 Nov 28;17(1):110.
- Amano H, Tanaka Y, Kawashima H, Deie K, Suzuki K, Fujiogi M, Morita K, Iwanaka T, Uchida H. Mesh hiatal reinforcement in laparoscopic Nissen fundoplication for neurologically impaired children is safe and feasible. Nagoya J Med Sci. 2017 Nov;79(4):427-433.
- Tanaka Y, Tainaka T, Sumida W, Shirota C, Murase N, Oshima K, Shirotsuki R, Chiba K, Uchida H. Comparison of outcomes of thoracoscopic primary repair of gross type C esophageal atresia performed by qualified and non-qualified surgeons. Pediatr Surg Int. 2017 Oct;33(10):1081-1086.
- Sumida W, Uchida H, Tanaka Y, Tainaka T, Shirota C, Murase N, Oshima K, Shirotsuki R, Chiba K. Review of redo-Kasai portoenterostomy for biliary atresia in the transition to the liver transplantation era. Nagoya J Med Sci. 2017 Aug;79(3):415-420.
- Makita S, Kaneko K, Ono Y, Uchida H. Risk factors for thoracic and spinal deformities following lung resection in neonates, infants, and children. Surg Today. 2017 Jul;47(7):810-814.
- Shirota C, Hinoki A, Takahashi M, Tanaka Y, Tainaka T, Sumida W, Murase N, Oshima K, Shirotsuki R, Chiba K, Morimoto Y, Uchida H. New Navigation Surgery for Resection of Lymphatic Malformations Using Indocyanine Green Fluorescence Imaging. Am J Case Rep. 2017 May 13;18:529-531.
- Shirota C, Tainaka T, Uchida H, Hinoki A, Chiba K, Tanaka Y. Laparoscopic resection of neuroblastomas in low- to high-risk patients without image-defined risk factors is safe and feasible. BMC Pediatr. 2017 Mar 14;17(1):71.
- Tainaka T, Uchida H, Tanano A, Shirota C, Hinoki A, Murase N, Yokota K, Oshima K, Shirotsuki R, Chiba K, Amano H, Kawashima H, Tanaka Y. Two-Stage Thoracoscopic Repair of Long-Gap Esophageal Atresia Using Internal Traction Is Safe and Feasible. J Laparoendosc Adv Surg Tech A. 2017 Jan;27(1):71-75.
- Oshima K, Uchida H, Tainaka T, Tanano A, Shirota C, Yokota K, Murase N, Shirotsuki R, Chiba K, Hinoki A. Left thoracoscopic two-stage repair of tracheoesophageal fistula with a right aortic arch and a vascular ring. J Minim Access Surg. 2017 Jan-Mar;13(1):73-75.
- 2016
- Yokota K, Uchida H, Tanano A, Shirota C, Tainaka T, Hinoki A, Murase N, Oshima K, Shirotsuki R, Chiba K. Steroid pulse therapy prevents restenosis following balloon dilatation for esophageal stricture. Pediatr Surg Int, 2016; 32: 875-879.
- Tanaka Y, Uchida H, Kawashima H, Fujiogi M, Suzuki K, Takazawa S, Deie K, Amano H, Iwanaka T. More than one-third of successfully nonoperatively treated patients with complicated appendicitis experienced recurrent appendicitis: Is interval appendectomy necessary? J Pediatr Surg, 2016.
- Tanaka Y, Kawashima H, Mori M, Fujiogi M, Suzuki K, Amano H, Morita K, Arakawa Y, Koh K, Oguma E, Iwanaka T, Uchida H. Contraindications and image-defined risk factors in laparoscopic resection of abdominal neuroblastoma. Pediatr Surg Int, 2016; 32: 845-850.
- Tainaka T, Uchida H, Tanano A, Shirota C, Hinoki A, Murase N, Yokota K, Oshima K, Shirotsuki R, Chiba K, Amano H, Kawashima H, Tanaka Y. Two-Stage Thoracoscopic Repair of Long-Gap Esophageal Atresia Using Internal Traction Is Safe and Feasible. J Laparoendosc Adv Surg Tech A, 2016.
- Shirota C, Uchida H, Ono Y, Murase N, Tainaka T, Yokota K, Oshima K, Shirotsuki R, Hinoki A, Ando H. Long-term outcomes after revision of Kasai portoenterostomy for biliary atresia. J Hepatobiliary Pancreat Sci, 2016.
- Oshima K, Uchida H, Tainaka T, Tanano A, Shirota C, Yokota K, Murase N, Shirotsuki R, Chiba K, Hinoki A. Left thoracoscopic two-stage repair of tracheoesophageal fistula with a right aortic arch and a vascular ring. J Minim Access Surg, 2016.
- Nakamura H, Murase N, Koga H, Cazares J, Lane GJ, Uchida H, Yamataka A. Classification of biliary atresia in the laparoscopic era. Pediatr Surg Int, 2016.
- Murase N, Uchida H, Seki T, Hiramatsu K. A feasibility of single-incision laparoscopic percutaneous extraperitoneal closure for treatment of incarcerated inguinal hernia in children: our preliminary outcome and review of the literature. Nagoya J Med Sci, 2016; 78: 19-25.
- Makita S, Kaneko K, Ono Y, Uchida H. Risk factors for thoracic and spinal deformities following lung resection in neonates, infants, and children. Surg Today, 2016.
- Kamei H, Ito Y, Onishi Y, Suzuki M, Imai H, Kurata N, Hori T, Tainaka T, Uchida H, Ogura Y. Cytomegalovirus (CMV) Monitoring After Liver Transplantation: Comparison of CMV Pp65 Antigenemia Assay with Real-Time PCR Calibrated to WHO International Standard. Ann Transplant, 2016; 21: 131-136.
- Deie K, Uchida H, Kawashima H, Tanaka Y, Fujiogi M, Amano H, Murase N, Tainaka T. Laparoscopic side-to-side pancreaticojejunostomy for chronic pancreatitis in children. J Minim Access Surg, 2016.
- Deie K, Uchida H, Kawashima H, Tanaka Y, Amano H, Murase N, Tainaka T. Operative procedures of single-incision laparoscopic repair of pediatric epigastric hernia have become simple and feasible with the use of a novel suture-assisting needle. J Ped Surg Case Reports, 2016; 4: 22-26.
- 2015
- Tanaka Y, Uchida H, Kawashima H, Sato K, Takazawa S, Deie K, Masuko T, Kanno K, Shimizu M. Influence of surgical intervention on neurodevelopmental outcome in infants with focal intestinal perforation. Pediatr Int, 2015.
- Tanaka Y, Uchida H, Kawashima H, Fujiogi M, Takazawa S, Deie K, Amano H. Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J Pediatr Surg, 2015.
- Takazawa S, Uchida H, Kawashima H, Tanaka Y, Sato K, Jimbo T, Iwanaka T. Laparoscopic partial gastrectomy of a huge gastric duplication cyst in an infant. Nagoya J Med Sci, 2015; 77: 291-296.
- Tainaka T, Uchida H, Ono Y, Tanano A, Shirota C, Yokota K, Murase N, Makita S, Shirotsuki R. A new modification of laparoscopic percutaneous extraperitoneal closure procedure for repairing pediatric femoral hernias involving a special needle and a wire loop. Nagoya J Med Sci, 2015; 77: 531-535.
- Shirota C, Uchida H. Initial treatment of septated parapneumonic empyema with drainage plus fibrinolytic agents is equally effective as video- assisted thoracoscopic surgery, and is suitable as first-line therapy. Transl Pediatr, 2015; 4: 41-44.
- Okuyama H, Koga H, Ishimaru T, Kawashima H, Yamataka A, Urushihara N, Segawa O, Uchida H, Iwanaka T. Current Practice and Outcomes of Thoracoscopic Esophageal Atresia and Tracheoesophageal Fistula Repair: A Multi-institutional Analysis in Japan. J Laparoendosc Adv Surg Tech A, 2015.
- Murase N, Uchida H, Tanano A, Shirota C, Hinoki A, Tainaka T, Yokota K, Oshima K, Shirotsuki R. Emergency hepatectomy for hepatic arteriovenous malformationcombined with pulmonary hypertension in an infant. J Ped Surg Case Reports, 2015; 3: 534-536.
- Murase N, Uchida H, Tainaka T, Kawashima H, Tanaka Y, Amano H, Kishimoto H. Laparoscopic-assisted pancreaticoduodenectomy in a child with gastrinoma. Pediatr Int, 2015; 57: 1196-1198.
- Murase N, Uchida H, Ono Y, Tainaka T, Yokota K, Tanano A, Shirota C, Shirotsuki R. A New Era of Laparoscopic Revision of Kasai Portoenterostomy for the Treatment of Biliary Atresia. Biomed Res Int, 2015; 2015: 173014.
- Murase N, Uchida H, Kaneko K, Ono Y, Makita S, Yokota K. Prophylactic effect of H2 blocker for anastomotic stricture after esophageal atresia repair. Pediatr Int, 2015; 57: 461-464.
- Murase N, Uchida H, Hiramatsu K. Accessory scrotum with perineal lipoma diagnosed prenatally: case report and review of the literature. Nagoya J Med Sci, 2015; 77: 501-506.
- Kawano Y, Suzuki M, Kawada J, Kimura H, Kamei H, Ohnishi Y, Ono Y, Uchida H, Ogura Y, Ito Y. Effectiveness and safety of immunization with live-attenuated and inactivated vaccines for pediatric liver transplantation recipients. Vaccine, 2015; 33: 1440-1445.
- Iwanaka T, Yamataka A, Uemura S, Okuyama H, Segawa O, Nio M, Yoshizawa J, Yagi M, Ieiri S, Uchida H, Koga H, Sato M, Soh H, Take H, Hirose R, Fukuzawa H, Mizuno M, Watanabe T. Pediatric Surgery. Asian J Endosc Surg, 2015; 8: 390-407.
- Fujiogi M, Tanaka Y, Kawashima H, Toma M, Suzuki K, Amano H, Morita K, Uchida H, Iwanaka T. An Easy and Safe Technique for Laparoscopic Pyloromyotomy: Using a Vascular Clamp for Stabilization of the Pylorus. J Laparoendosc Adv Surg Tech A, 2015.
- Amano H, Uchida H, Kawashima H, Deie K, Murase N, Makita S, Yokota K, Tanaka Y. The umbilical benz incision for reduced port surgery in pediatric patients. JSLS, 2015; 19.
- 2014
- Yokota K, Uchida H, Kaneko K, Ono Y, Murase N, Makita S, Hayakawa M. Surgical complications, especially gastroesophageal reflux disease, intestinal adhesion obstruction, and diaphragmatic hernia recurrence, are major sequelae in survivors of congenital diaphragmatic hernia. Pediatr Surg Int, 2014; 30: 895-899.
- Tanaka Y, Uchida H, Kawashima H, Masuko T, Takazawa S, Deie K, Amano H, Iwanaka T. Laparoscopic partial nephrectomy for the treatment of large cystic nephroma in children. J Laparoendosc Adv Surg Tech A, 2014; 24: 901-906.
- Takazawa S, Uchida H, Kawashima H, Tanaka Y, Sato K, Jimbo T, Deie K, Koiwai K, Nomura K, Iwanaka T. Massive hemorrhage after Kasai portoenterostomy in a patient with a congenital extrahepatic portosystemic shunt, malrotation and a double aortic arch: report of a case. Surg Today, 2014; 44: 1561-1564.
- Takazawa S, Uchida H, Kawashima H, Tanaka Y, Masuko T, Deie K, Amano H, Kobayashi K, Tada M, Iwanaka T. Urethroscopic holmium: YAG laser ablation for acquired posterior urethral diverticulum after repair of anorectal malformations. Pediatr Surg Int, 2014.
- Amano H, Uchida H, Kawashima H, Tanaka Y, Kishimoto H. Full-thickness small intestine necrosis with midgut volvulus, distributed in a patchy fashion, is reversible with moderate blood flow: resumption of normal function to non-viable intestine. Nagoya J Med Sci, 2014; 76: 375-380.
- 2013
- Yoshida M, Matsuoka K, Nakazawa A, Yoshida M, Inoue T, Kishimoto H, Nakayama M, Takaba E, Hamazaki M, Yokoyama S, Horie H, Tanaka M, Gomi K, Ohama Y, Kigasawa H, Kitano Y, Uchida H, Kanamori Y, Iwanaka T, Tanaka Y. Sacrococcygeal yolk sac tumor developing after teratoma: a clinicopathological study of pediatric sacrococcygeal germ cell tumors and a proposal of the pathogenesis of sacrococcygeal yolk sac tumors. J Pediatr Surg, 2013; 48: 776-781.
- Tanaka Y, Uchida H, Kawashima H, Sato K, Takazawa S, Masuko T, Deie K, Iwanaka T. Complete thoracoscopic versus video-assisted thoracoscopic resection of congenital lung lesions. J Laparoendosc Adv Surg Tech A, 2013; 23: 719-722.
- Tanaka Y, Uchida H, Kawashima H, Sato K, Takazawa S, Jimbo T, Iwanaka T. Successful two-stage thoracoscopic repair of long-gap esophageal atresia using simple internal traction and delayed primary anastomosis in a neonate: report of a case. Surg Today, 2013; 43: 906-909.
- Takazawa S, Uchida H, Kawashima H, Tanaka Y, Sato K, Jimbo T, Masuko T, Deie K, Iwanaka T. Minimally invasive surgery for pediatric cases of large extraovarian teratoma with considerable solid component. J Pediatr Surg, 2013; 1: 226-229.
- Takazawa S, Uchida H, Kawashima H, Tanaka Y, Masuko T, Deie K, Nagase Y, Iwanaka T. External stabilization for severe tracheobronchomalacia using separated ring-reinforced ePTFE grafts is effective and safe on a long-term basis. Pediatr Surg Int, 2013; 29: 1165-1169.
- Masuko T, Uchida H, Kawashima H, Tanaka Y, Deie K, Iwanaka T. Laparoscopic excision of urachal remnants is a safe and effective alternative to open surgery in children. J Laparoendosc Adv Surg Tech A, 2013; 23: 1016-1019.
- Kato M, Koh K, Oshima K, Oguma E, Uchida H, Kishimoto H, Kikuchi A, Hanada R. Long-term survivor of relapsed stage IV malignant rhabdoid tumor of the kidney. Pediatr Int, 2013; 55: 245-248.
- Ishimaru T, Takazawa S, Uchida H, Kawashima H, Fujii M, Harada K, Sugita N, Mitsuishi M, Iwanaka T. Development of a needle driver with multiple degrees of freedom for neonatal laparoscopic surgery. J Laparoendosc Adv Surg Tech A, 2013; 23: 644-648.
- Deie K, Uchida H, Kawashima H, Tanaka Y, Masuko T, Takazawa S. Single-incision laparoscopic-assisted appendectomy in children: exteriorization of the appendix is a key component of a simple and cost-effective surgical technique. Pediatr Surg Int, 2013; 29: 1187-1191.
- Japanese multicenter study group on male high imperforate anus, Yamataka A, Morikawa Y, Yagi M, Kimura O, Kuroda T, Ueno S, Iwanaka T, Iwai J, Zaizen Y, Koga H, Shimono R, Yagi M, Kubota M, Murase N, Kanamori Y, Tanaka H, Takahashi M, Ikeda T, Kubota A, Nara K, Satoh K, Amano H, Takazawa S, Tanaka Y, Uchida H, Kawashima H, Jimbo T, Fukumoto K, Ueno S, Ishimaru T. Multicenter retrospective comparative study of laparoscopically assisted and conventional anorectoplasty for male infants with rectoprostatic urethral fistula. J Pediatr Surg, 2013; 48: 2383-2388.
Research Keywords
Pediatric endoscopic surgery, Minimally invasive surgery, Biliary atresia, Congenital biliary dilatation, Congenital esophageal atresia, Congenital diaphragmatic hernia, Neonatal surgery, Childhood cancer