Laboratories
- Back
- Top > Laboratories > Internal Medicine > Nephrology
Internal MedicineNephrology
Introduction
Department of nephrology has been established since Jan.2002, when Dr. Seiichi Matsuo was elected as the first chief professor. When Prof. Matsuo appointed as the director of Nagoya University Hospital on Apr.2010, associate professor Shoichi Maruyama was appointed as the extraordinary professor, and then he was elected as chief professor on Apr.2015 after president appointed of Prof. Matsuo. Our department consists of 10 faculty members(Prof. Maruyama, 2 lecturers, 1 assistant professor, 3 assistant clinical professors, 2 designated lecturers and 1 designated assistant professor), 5 staff doctors, 1 senior resident, 25 graduate school student including 2 students from abroad, 7 fellow studying abroad, 5 visiting researchers. Department of renal replacement therapy established on Feb.2005 consists of 3 faculty members (professor, associate professor and assistant professor) and acts in clinical and research aspects for peritoneal dialysis. Moreover, department of CKD initiatives established since 2008 consists of 3 faculty members (1 designated associate professor ,2 designated assistant professors) engaged in enlightenment and research for patients with chronic kidney deasese (CKD). Total 57 members strive to promote three major affairs of ①clinical②education③research in nephrology field.
Research Projects
1. 『Development of novel cell therapy for kidney diseases by administration of adipose tissue-derived mesenchymal stem cells』
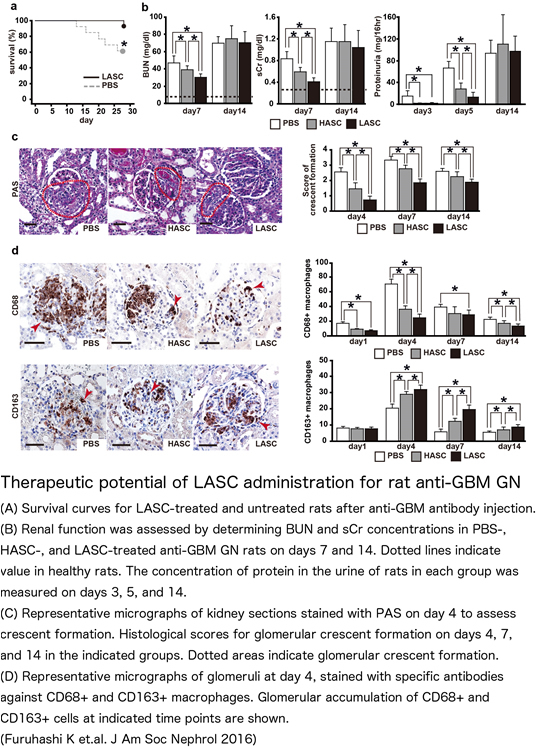
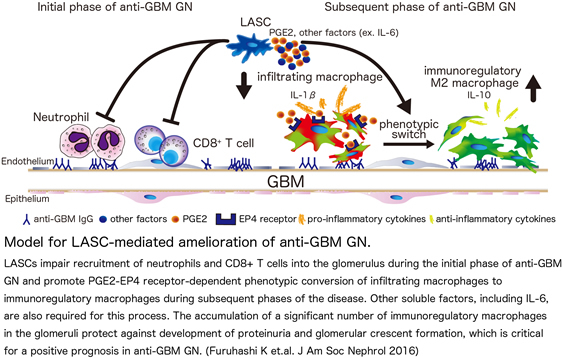
Mesenchymal stem cells (MSCs) have the capacity to differentiate into multiple mesenchymal lineages, including osteoblasts, chondrocytes, and adipocytes. Apart from the classic regenerative property of MSCs, mounting evidence from studies for MSCs suggests that MSCs can modulate inflammatory immune responses. Our laboratory have focused on adipose tissue-derived MSCs (ASCs) because ASCs have a number of practical advantages over BM-MSCs relating to their abundance and availability. For cell transfer therapy, a reduction in the concentration of serum in MSC cultures is beneficial for recipients because this reduces concerns about infection with microorganisms or pathogenic proteins originating from culture media. Human ASCs grown under low-serum conditions (LASCs) display comparable growth to human BM-MSCs cultured in 20% serum media. Of further interest, human LASCs more effectively produce growth factors and Immunoregulatory factors than ASCs grown under high-serum conditions (HASCs).
Rapidly progressive glomerulonephritis (RPGN) characterized by poor prognosis is still intractable glomerulonephritis. The therapeutic options for RPGN has been limited in corticosteroid and cyclophosphamide that causes adverse effect including infection and cytotoxicity. We systemically administered adipose-derived stromal cells (ASCs) in a rat model of RPGN and found that this treatment protected against renal injury (Furuhashi K, J Am Soc Nephrol 2013). We have demonstrated significant therapeutic potential of LASC administration also in other rodent models of acute kidney injury, peritonitis and wound healing. Based on results from animal studies, we are currently investigating for clinical application of LASC therapy including cell preparation and assessment of safety.
2. 『Elucidation of onset/development of renal diseases through immunological mechanisms』
i) “Roles of immuneregulatory M2 macrophages in renal diseases”
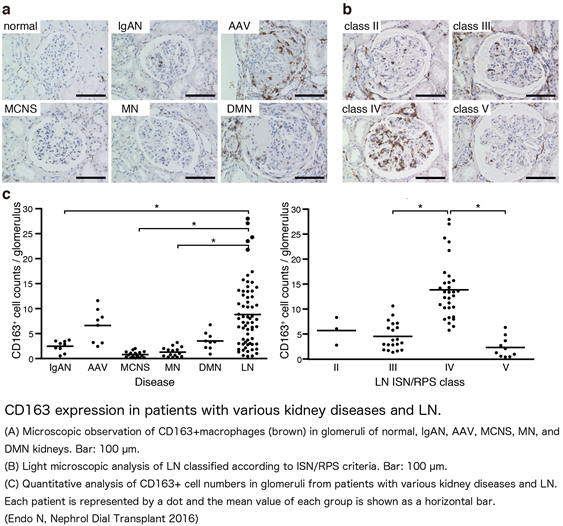
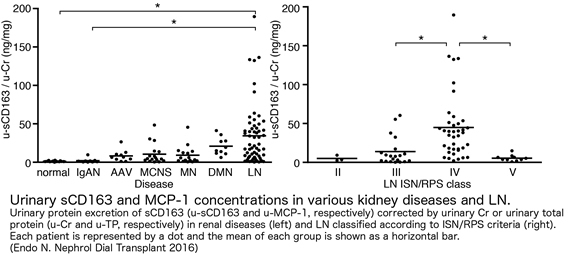
Macrophages, which are scavenger leukocytes to phagocytose and process harmful foreign particles in a living body, are well known to induce tissue inflammation after excessive cell activation. In addition to classically activated macrophages playing effector roles in tissue injury (M1 macrophages), alternatively activated M2 macrophages are recently identified to involve in the resolution of inflammation on the process of tissue repair. Our laboratory stained CD206+ macrophages on kidney biopsy samples from patients with various kidney diseases, and histologically analyzed the differences of M2 macrophage accumulation. We clearly demonstrated dominant accumulation of CD206+ macrophages in glomeruli with ANCA-associated glomerulonephritis often inducing rapidly progressive glomerulonephritis in clinical and active lupus nephritis (class IV) complicated with systemic lupus erhythematosus. (Endo N, Nephrol Dial Transplant 2016)。
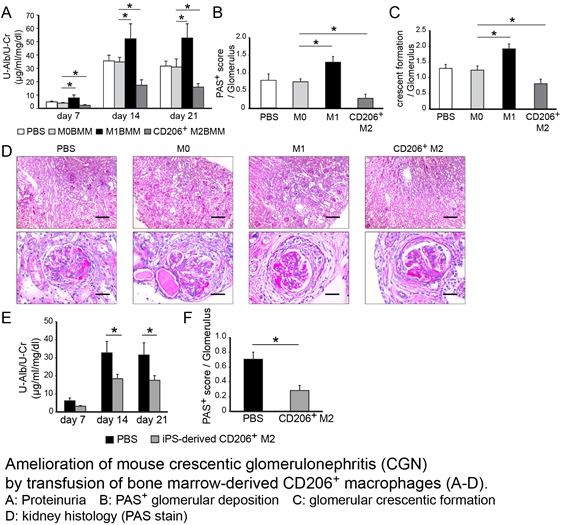
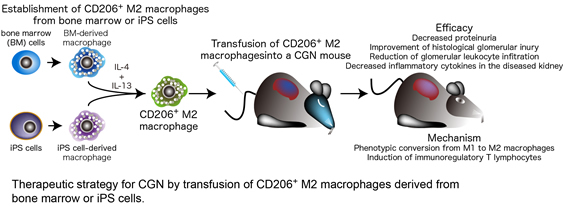
On another insight for roles of M2 macrophage in kidney diseases, we demonstrated that transfusion of immunoregulatory M2 macrophages derived from bone marrow or induced pluripotent stem cells could ameliorate CGN. The M2 macrophage-driven phenotypic conversion from inflammatory macrophages to M2 cells and the induction of immunoregulatory T lymphocytes were involved in the therapeutic mechanism. This study suggests M2 macrophage transfusion as a novel therapeutic option for CGN.
ii)“Development of novel biomarkers for kidney diseases by using leukocyte expressing proteins”
Histological evaluation on kidney samples, combined with screening examination including serum creatinine and urine analysis, is one of the essential examination for precise diagnosis, assessment of disease activity and treatment planning in kidney diseases. However, physical burden involved in the procedure of kidney biopsy makes repeated examination unrealistic. Therefore, useful biomarkers for therapy evaluation, judgement of recurrent illness and prediction of the disease prognosis are currently desirable in clinical field. Our laboratory aimed to develop specific biomarkers for glomerulonephritis and identified several candidate molecules. CD163, that acts as a scavenger receptor for the hemoglobin-haptoglobin complex, is actively shed from the plasma membrane in response to certain inflammatory stimuli including LPS and oxidative stress. We recently analyzed urine and kideney samples from 74 lupus nephritis patients in Nagoya Kidney Disease Registration (N-KDR) from 2009 to 2012, and revealed that urinary sCD163 level was strongly correlated with glomerular CD163+ cell counts and histological disease activity (Endo N, Nephrol Dial Transplant 2016). Our findings in the study indicate that urinary sCD163 level can serve as a biomarker for macrophage-dependent glomerular inflammation in human LN. We now attempt to validate the clinical significance of CD163 in large-scale patient population, and are investigating other candidate molecules for biomarkers.
3. 『The glycosylated transmembrane protein CD147/basigin in the kidneys』
The glycosylated transmembrane protein CD147/basigin, also known as extracellular matrix metalloproteinase (MMP) inducer (EMMPRIN), contributes to cell survival, migration and cancer invasion. In normal kidneys, high expression of CD147 is detected in tubular epithelial cells (TECs). The pathophysiological roles of CD147 in the kidneys are diverse, ranging from involvement in the occurrence of acute kidney injury (AKI) that is frequently accompanied by ischemia, inflammation and a loss of self-tolerance to the progression of chronic kidney disease (CKD). In AKI induced by ischemia, it is the CD147 on neutrophils, rather than that on TECs, that coordinately participates in massive neutrophil recruitment via acting as a physiological ligand for E-selectin, which is specifically enhanced in the endothelium upon inflammatory stimulation. Whereas CD147 thus plays deleterious roles in ischemic and fibrotic kidney injuries, CD147 expression on lymphocytes decreases the disease activity of lupus nephritis (LN) by functioning as a potential negative regulator of the extraordinary proliferation of interleukin-17 producing T cells that occurs in this disease. In line with these basic studies, our clinical data indicate the potential of plasma CD147 to function as a critical biomarker for both ischemic AKI and LN. Multidisciplinary research regarding CD147 functions may open a new avenue for targeting therapeutics for kidney diseases.
4. 『Midkine and the kidney: health and diseases』
Midkine (MK; gene name, Mdk),a heparin-binding growth factor, regulates cell growth, cell survival, migration and anti-apoptotic activity in nephrogenesis and development. In the kidney, MK is expressed mainly in proximal tubular epithelial cells, and is induced by oxidative stress through the activation of hypoxia-inducible factor-1α. The pathophysiological roles of MK are diverse, ranging from the occurrence of acute kidney injury (AKI) to progression of chronic kidney disease, often accompanied by hypertension, renal ischemia and diabetic nephropathy. In particular, MK regulates BP through Cytochrome P450-Derived Eicosanoids. Such multidisciplinary findings may open new avenues for targeting therapies for hypertension and various renal diseases, including AKI and diabetic nephropathy.
5. 『The development of metabolic syndrome and chronic kidney diseases (CKD) via fructose metabolism』
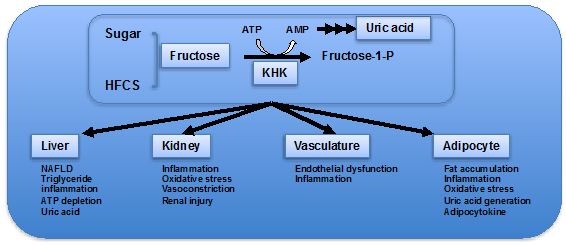
Intake of fructose such as from sucrose and high fructose corn syrup (HFCS) has increased dramatically in the last hundred years, and epidemiologically linked with the increase of metabolic syndrome (obesity, hypertension, diabetes, dyslipidemia, NAFLD), and CKD. However, the causative role of fructose metabolism and its mechanism for the development of these disorder and renal injury is still unclear. Fructose is primarily metabolized by fructokinase (ketohexokinase, KHK) which exists in two isoforms, KHK-C and KHK0A. KHK-C expressed in the liver, kidney and intestines, and KHK-A expressed ubiquitously. In collaboration with Prof. Richard J Johnson at Division of Renal Diseases and Hypertension, University of Colorado, we have reported that fructose-induced obesity and insulin resistance, dyslipidemia, NAFLD, and aging-associated kidney disease are prevented in mice lacking both KHK-C and KHK-A. Currently, we are continuing the investigation to clarify the role of fructose metabolism and uric acid generation in the metabolic syndrome including hypertension and diabetes and CKD to establish the therapy against these diseases.
6. 『Exosomes and micro RNA research』
i)“Diagnostic biomarker development using plasma exosomes”
In general, biopsy is a powerful diagnostic tool for kidney diseases. But our final goal is to know the kidney condition in real time, which is always changing depending on the disease activity and therapy.
Exosomes are small (30-150nm) membrane vesicles of endosomal origin that contain host cell's proteins, mRNAs, and microRNAs (miRNAs). Especially in cancer researching field, they have gotten a lot of attention for ideal biomarker. On the other hands, exosomes found in blood can originate from any tissue or cell types, so it is sometimes difficult to detect small changes in exosomes from target organ. Now, we developed the new system which makes it possible to collect exosomes of interesting. We focus on exosomes from kidney mesangial cells.
ii)“Nucleic acid medicine”
During past years, tremendous efforts have been made to create new class of molecular target pharmaceutical. Nucleic acid medicines are one of them. Out of those, we are focusing on microRNAs (miRNAs). Different from other artificial nucleic acids, miRNAs are synthesized endogenously, and work as fine-tuners of gene expressions. With proper drug delivery systems, giving miRNA exogenous manner could suppress molecular cascades safely. Now we are working on the treatment of septic acute kidney injury (Septic AKI) with miRNAs. In the future, we would like to develop the tailored therapy by choosing therapeutic miRNAs depending on the disease activity or phases.
7. 『Clinical research』
i)“Nagoya Nephrology Research Consortium”
We founded a new comprehensive study plan, NNRC(Nagoya Nephrology Research Consortium) as a substitute for N-KDR which was operated from 2011.We intended to build renal disease registration system to recruit patients and collect specimens.
ii)“Cohort of the medical examination”
The purpose of this study is risk estimation of lifestyle diseases using genetic analysis. We clarify the risk of lifestyle diseases and stratify the risk for each predisposition by combination analysis between individual genetic information and lifestyle information. We collect health examination data, lifestyle information evaluated using self-administered questionnaires, genetic information which are related to lifestyle diseases, and the meal purchase data which were automatically recorded dietary elements when an employee buys lunch in the cafeteria.
iii)”Bibriography”
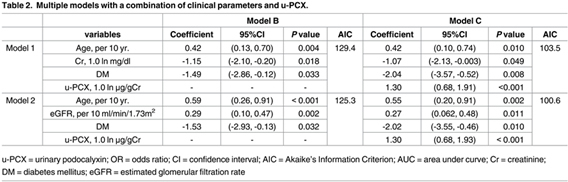
Imaizumi T, Nakatochi M, Akiyama S, Yamaguchi M, Kurosawa H, Hirayama Y, et al. Urinary Podocalyxin as a Biomarker to Diagnose Membranous Nephropathy. PLoS One, 2016; 11: e0163507.
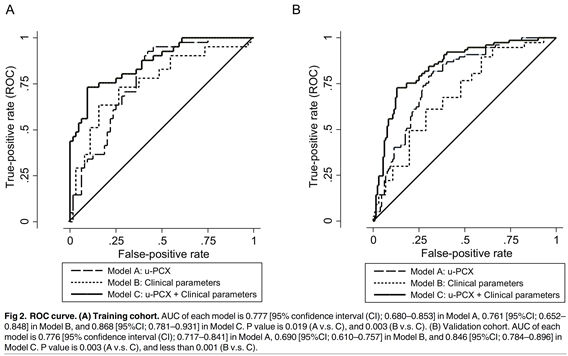
【Patients】
To construct the validation cohort, we extracted 358 consecutive NS cases from 1274 kidney biopsies between January 2012 and December 2013. After excluding cases where urine samples were not obtained or those who received immunosuppression treatment at the time of kidney biopsy, 209 NS cases were included.
【Conclusions】
In this study, we demonstrated the utility of u-PCX as a diagnostic marker for MN and the clinical usefulness of the diagnostic models, through the combination of u-PCX and clinical parameters including age, glomerular filtration rate, and diabetes mellitus.
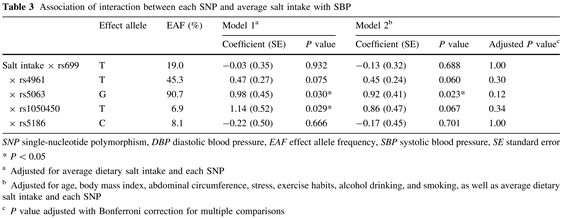
Imaizumi T, Ando M, Nakatochi M, Maruyama S, Yasuda Y, Honda H, et al. Association of interactions between dietary salt consumption and hypertension-susceptibility genetic polymorphisms with blood pressure among Japanese male workers. Clin Exp Nephrol. 2016; Aug 1.
【Patients】
This study is part of an ongoing observational prospective cohort study investigating metabolic syndrome and chronic kidney disease among male Japanese. Study participants were eligible for inclusion in this study if meal data were available. Analysis using SNP data was performed among those who consented to DNA sampling. Finally, the sample for this study was restricted to 2728 individuals who provided consent for the study protocol (including SNP typing) and whose meal purchase data were available.
【Conclusions】
The effect of salt consumption on BP differed by genotype. Dietary salt consumption and genetic variation can predict a high risk of hypertension.
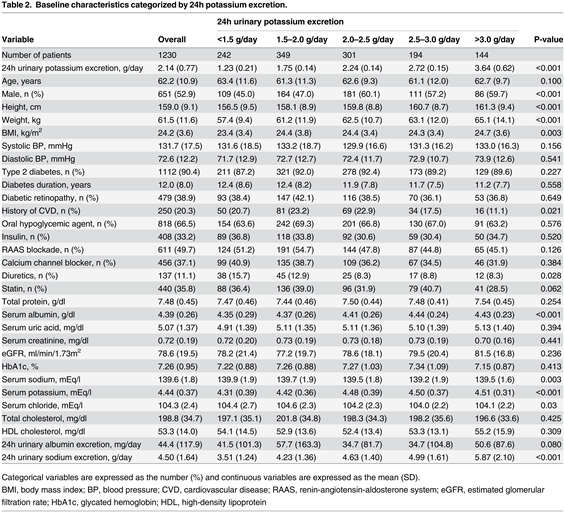
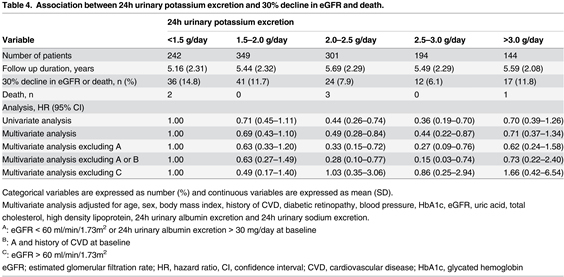
Nagata T, Sobajima H, Ohashi N, Hirakawa A, Katsuno T, Yasuda Y, et al. Association between 24h Urinary Sodium and Potassium Excretion and Estimated Glomerular Filtration Rate (eGFR) Decline or Death in Patients with Diabetes Mellitus and eGFR More than 30 ml/min/1.73m2. PLoS One, 2016; 11: e0152306.
【Patients】
This was a retrospective and observational cohort study at a single diabetes center in Ogaki Municipal Hospital, Ogaki, Japan. A total of 4184 patients were screened for this study, and 1230 eligible patients were finally included and analyzed.
【Conclusions】
24h urinary sodium excretion was not significantly associated with a risk of 30% decline in eGFR or death in patients with diabetes. However, an increased risk of 30% decline in eGFR or death was significantly associated with 24h urinary potassium excretion < 1.5g/day than with 2.0-2.5 g/day and 2.5-3.0 g/day.
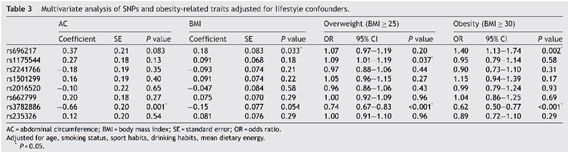
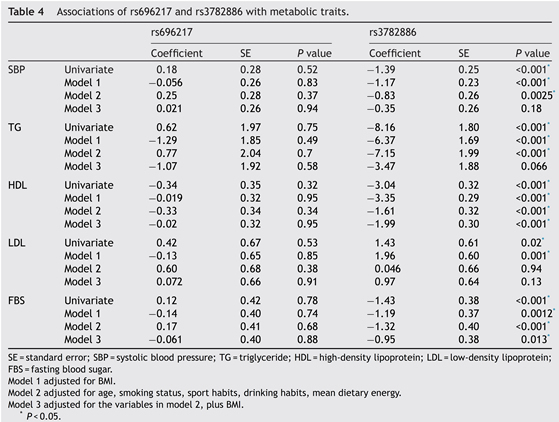
Imaizumi T, Ando M, Nakatochi M, Yasuda Y, Honda H, Kuwatsuka Y, et al. Effect of dietary energy and polymorphisms in BRAP and GHRL on obesity and metabolic traits.
Obes Res Clin Pract. 2016 May 27.
【Patients】
In this retrospective observational study. Only those who consented to DNA sampling were included, and the DNA samples were obtained between 2011 and 2014 from 5112 individuals. We did not provide any exclusion criteria. Any individuals who received the annual health examination were included in this research regardless of health problem.
【Conclusions】
Average dietary energy in lunch, rs3782886, and rs696217 were associated with obesity, and rs3782886 was associated with other metabolic abnormalities.
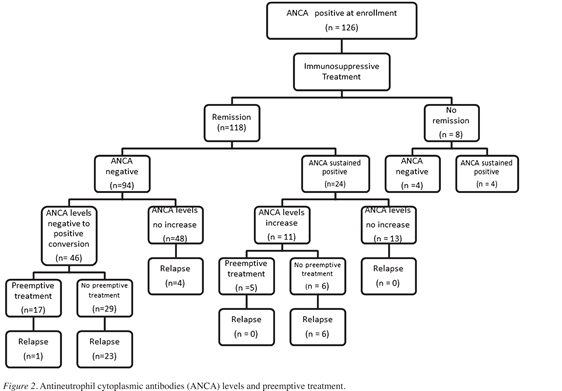
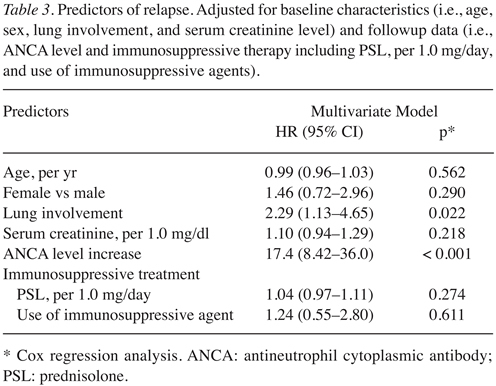
Yamaguchi M, Ando M, Kato S, Katsuno T, Kato N, Kosugi T, et al. Increase of Antimyeloperoxidase Antineutrophil Cytoplasmic Antibody (ANCA) in Patients with Renal ANCA-associated Vasculitis: Association with Risk to Relapse. J Rheumatol. 2015; 42: 1853-60.
【Patients】
Our cohort study included patients aged > 15 years diagnosed with AAV including GPA and MPA on the basis of the European Medicines Agency algorithm23 with a consensus methodology for the classification of the AAV between January 2004 and December 2012. Of 131 such patients, we excluded 5 (3.8%) because of a history of malignancies (n = 1), missing data (n = 1), a lack of immunosuppressive therapy (n = 2), or ANCA-negative test results at the time of initial visit (n = 1). Finally, 126 patients with AAV (93.3%) who received immunosuppressive therapy were included.
【Conclusions】
In our study, an increase in ANCA level during remission was associated with a risk of disease relapse. A rise in ANCA level may be useful for guiding treatment decisions in appropriate subsets of patients with ANCA-associated vasculitis.
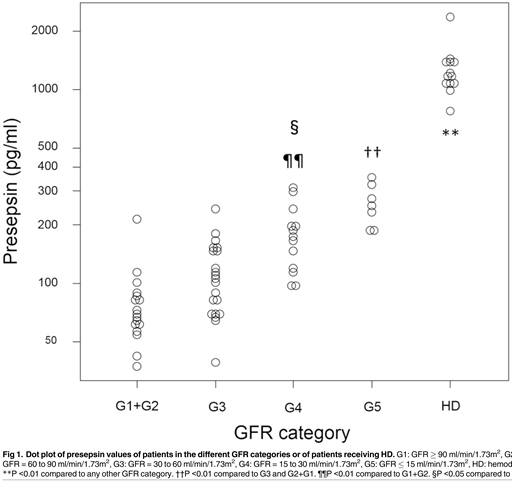
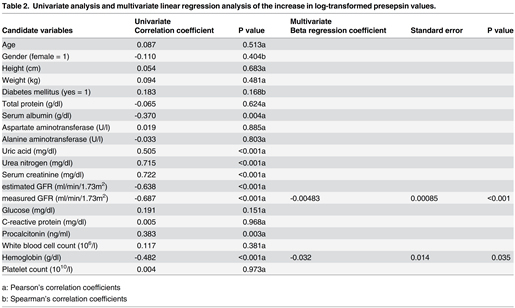
Nagata T, Yasuda Y, Ando M, Abe T, Katsuno T, Kato S, et al. Clinical impact of kidney function on presepsin levels. PLoS One, 2015; 10: e0129159.
【Patients】
Patients who were not receiving HD were included if they had undergone inulin renal clearance measurements for the accurate measurement of GFR (measured GFR), and patients who were receiving hemodialysis (HD) were included if they had anuria. Exclusion criteria were infection, cancer, liver disease, autoimmune disorders, or steroid or immunosuppressant use. Finally, seventy-one patients were included.
【Conclusions】
Presepsin levels were markedly high in patients receiving HD, similar to values seen in patients with severe sepsis or septic shock. In patients who were not receiving HD, presepsin levels increased as GFR decreased. Thus, the evaluation of presepsin levels in patients with chronic kidney disease requires further consideration, and a different cutoff value is needed for diagnosing sepsis in such patients. We found that measured GFR and hemoglobin levels were significantly associated with elevated presepsin levels.
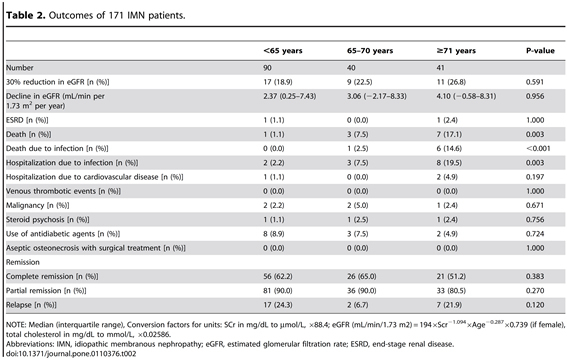
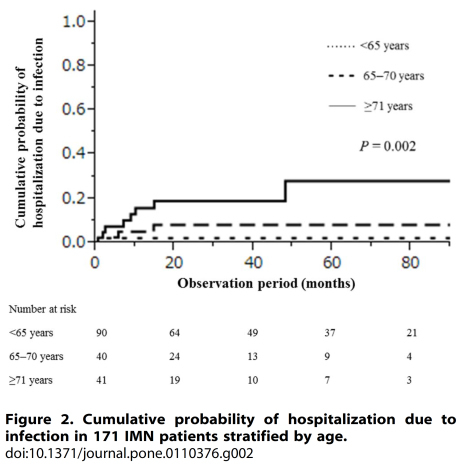
Yamaguchi M, Ando M, Yamamoto R, Akiyama S, Kato S, Katsuno T, et al. Patient age and the prognosis of idiopathic membranous nephropathy. PLoS One, 2014; 9:e110376.
【Patients】
We recruited 171 Japanese patients with IMN, including 90 (52.6%) patients, 65 years old, 40 (23.4%) patients 65-70 years, and 41 (24.0%) patients 71 years. Clinical characteristics and outcomes were compared between younger and older IMN patients.
【Conclusions】
Younger and older IMN patients had similar renal outcomes. However, older patients were more likely to develop infection when using immunosuppressants. Patients with a poor response in the first month following the initiation of immunosuppressive therapy should be carefully monitored for infection and may require a faster prednisolone taper.
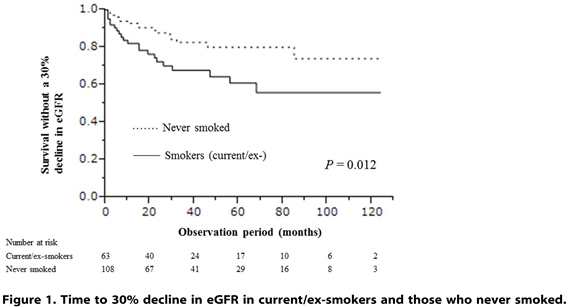
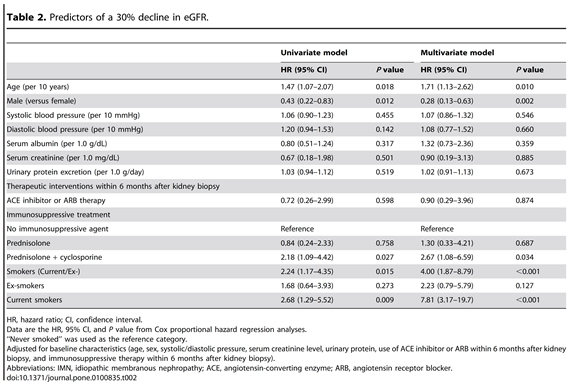
Yamaguchi M, Ando M, Yamamoto R, Akiyama S, Kato S, Katsuno T, et al. Smoking is a risk factor for the progression of idiopathic membranous nephropathy. PLoS One, 2014; 9: e100835.
【Patients】
This study used the Nagoya Nephrotic Syndrome Cohort Study (N-NSCS), including 171 patients with idiopathic membranous nephropathy (IMN) from 10 nephrology centers in Japan. The dose-response relationships between cigarette smoking and the outcomes were assessed by using multivariate Cox proportional hazards models adjusted for clinically relevant factors. The primary outcome was a 30% decline in the estimated glomerular filtration rate (eGFR). The secondary outcome was first complete remission (CR) of proteinuria.
【Conclusions】
Smoking is a significant and dose-dependent risk factor for IMN progression. All patients with IMN who smoke should be encouraged to quit.
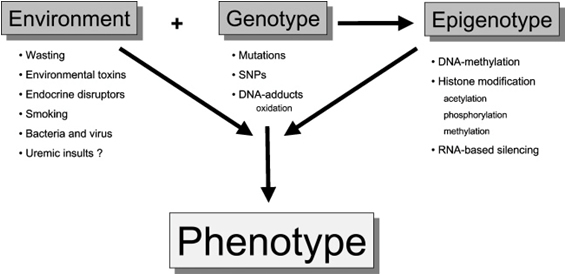
8. 『Association between immune dysfunction due to uremia and outcomes in chronic kidney disease』
Patients with chronic kidney disease (CKD) have increased mortality from cardiovascular disease (CVD) and infection. Of note, protein-energy wasting (PEW) and persistent inflammation are strongly associated with these complications in CKD stage5 patients. We have investigated that potential links between the immune dysfunction in uremia, inflammation, infection and increased risk of atherosclerosis and CVD. Then, we have hypothesized that an immunosuppressed state, leading to increased susceptibility to infection, may lead to chronic inflammation and that inflammation may also ensue as a consequence of a state of immune-activation. In addition, external factors, such as the dialysis procedure, dialysis access (blood or peritoneal) infections, medication, and PEW, may activate or inhibit the immune system (Figure 1). In order to work out a new strategy to improve the premature mortality of CKD patients, we have been conducting "NISE study (Nagoya Immunity System in End-stage renal disease study)", which is a prospective cohort study on Japanese CKD patients including 300 dialysis patients undergoing treatment in our affiliated hospitals. The aim of NISE study is to clarify if immune dysfunction in uremia affects CVD risk factors, infection rates and mortality in Japanese CKD patients. Especially, we have focused on alterations in genotype (SNPs), epigenotype (DNA methylation), and their environment in these patients (Figure 2). Moreover, we have also focused on cellular senescence (telomere attrition). The reports on NISE study have been published in international journals; ①association between DNA hyper-methylation and inflammatory markers (Nephron Extra 2:159-168, 2012), ②telomere attrition and elongation (Blood Purification 2016;41:25-33), ③neutrophil/lymphocyte ratio as a predictor of cardiovascular events (Clin Exp Nephrol 19:718-724, 2015), ④association between high ferritin level, malnutrition and infection-related hospitalization (Blood Purification 2016;42(1):56-63).
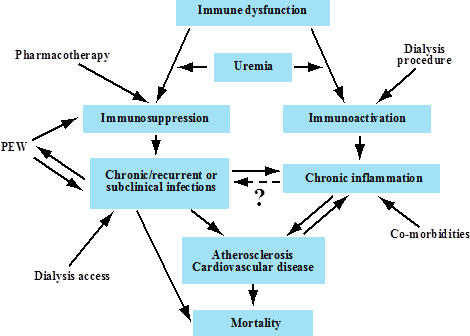
Figure 1. Immune dysfunction in uremia: Possible associations with infections and inflammation.
Kato S et al (Clin J Am Soc Nephrol 3:1526-1533, 2008)
9. 『Randomized control trial for the assessment of the anti-albuminuric effects of topiroxostat in hyperuricemic patients with diabetic nephropathy (the ETUDE study)』
Proteinuria is an established risk factor for diabetic nephropathy. The aim of this study was to assess whether topiroxostat, xanthine a selective oxidase inhibitor (XOi), reduces albuminuria in hyperuricemic patients with diabetic nephropathy and overt proteinuria. The ETUDE study is an ongoing 24-week, multicenter, open-label, randomized, parallel group study involving hyperuricemic patients with diabetic nephropathy. Patients are randomly assigned to high dose (topiroxostat 160 mg daily) or low dose (topiroxostat 40 mg daily). The primary endpoint is the change in albuminuria indicated after 24 treated weeks relative to the baseline values.
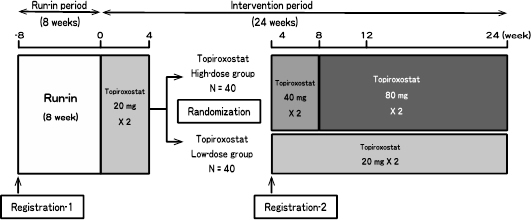
The flowchart of ETUDE study
10. 『Membranous nephropathy; development of diagnostics, elucidation of pathogenesis, clinical survey』
Membranous nephropathy (MN) is a leading cause of nephrotic syndrome in adults. It is classified as either primary (pMN) or secondary (sMN) depending on its etiology. MN is characterized by immune complex deposition in the subepithelial space of glomerular capillaries. In 10-20 % of patients, MN is associated with an underlying disease, such as autoimmune disease (e.g., systemic lupus erythematosus), infection, drugs and malignancies. When no underlying cause is identified, the disease is classified as primary (idiopathic). Therefore, the primary MN is diagnosed by exclusion.
It has long been suspected that primary MN is evoked by the in situ formation of immune complexes as circulating antibodies react with a podocyte antigen. In 2009, M-type phospholipase A2 receptor (PLA2R) was identified as a target podocyte antigen in primary MN. Circulating autoantibody against PLA2R were found in patients with idiopathic MN, but not in those with sMN or other glomerular diseases. The circulating anti-PLA2R autoantibody is useful biomarker for differential diagnosis of pMN. Moreover, it is being recognized that the level of circulating anti-PLA2R autoantibody correlated with clinical disease activity, precede corresponding changes in disease activity, and is useful indicator for a monitoring response to treatment and a prognosis assessment.
Our research project about anti-PLA2R antibody in Japanese patients with MN lunched in 2009. To this day, we had been trying and achieving to develop measurement methods of anti-PLA2R antibody, to develop in vitro and in vivo biological experiment platforms to dissolve a mechanism of pathogenesis in PLA2R associated MN, to research a prevalence of anti-PLA2R antibody in Japanese patients, to survey clinical and epidemiological situations in Japan. We first reporteded that the prevalence of anti-PLA2R antibodies in Japanese patients with pMN is approximately 50 %, which was lower than reports from China, Korea, USA, and European countries1). The anti-PLA2R antibody was not found in any Japanese patients without pMN.
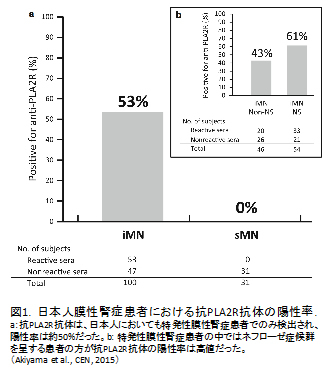
Currently we are operating several originally developed assay methods for anti-PLA2R antibody and commercial kits from EUROIMMUN AG company. We have much experience regarding measurement of anti-PLA2R antibody, therefore, we can provide measurement of anti-PLA2R antibody and technical support of methodology of anti-PLA2R antibody. Of course, we welcome your proposals of joint research. If you interested in our anti-PLA2R antibody and MN research project, please contact Shin'ichi Akiyama or Shoichi Maruyama.
Bibliography
- 2016
- Kato H, Nangaku M, Hataya H, Sawai T, Ashida A, Fujimaru R, Hidaka Y, Kaname S, Maruyama S, Yasuda T, Yoshida Y, Ito S, Hattori M, Miyakawa Y, Fujimura Y, Okada H, Kagami S, Joint Committee for the Revision of Clinical Guides of Atypical Hemolytic Uremic Syndrome in J. Clinical guides for atypical hemolytic uremic syndrome in Japan. Pediatr Int, 2016; 58: 549-555.
- Kato S, Ando M, Mizukoshi T, Nagata T, Katsuno T, Kosugi T, Tsuboi N, Maruyama S. Randomized control trial for the assessment of the anti-albuminuric effects of topiroxostat in hyperuricemic patients with diabetic nephropathy (the ETUDE study). Nagoya J Med Sci, 2016; 78: 135-142.
- Kato S, Shiels PG, McGuinness D, Lindholm B, Stenvinkel P, Nordfors L, Qureshi AR, Yuzawa Y, Matsuo S, Maruyama S. Telomere Attrition and Elongation after Chronic Dialysis Initiation in Patients with End-Stage Renal Disease. Blood Purif, 2016; 41: 25-33.
- Kubota K, Hoshino J, Ueno T, Mise K, Hazue R, Sekine A, Yabuuchi J, Yamanouchi M, Suwabe T, Kikuchi K, Sumida K, Hayami N, Sawa N, Takaichi K, Fujii T, Ohashi K, Akiyama S, Maruyama S, Ubara Y. Phospholipase A2 Receptor-Positive Idiopathic Membranous Glomerulonephritis with Onset at 95 Years: Case Report. Case Rep Nephrol Dial, 2016; 6: 76-82.
- Maeda K, Enomoto A, Hara A, Asai N, Kobayashi T, Horinouchi A, Maruyama S, Ishikawa Y, Nishiyama T, Kiyoi H, Kato T, Ando K, Weng L, Mii S, Asai M, Mizutani Y, Watanabe O, Hirooka Y, Goto H, Takahashi M. Identification of Meflin as a Potential Marker for Mesenchymal Stromal Cells. Sci Rep, 2016; 6: 22288.
- Mizuno M, Ito Y, Suzuki Y, Sakata F, Saka Y, Hiramatsu T, Tamai H, Mizutani M, Naruse T, Ohashi N, Kasuga H, Shimizu H, Kurata H, Kurata K, Suzuki S, Kido S, Tsuruta Y, Matsuoka T, Horie M, Maruyama S, Matsuo S. Recent analysis of status and outcomes of peritoneal dialysis in the Tokai area of Japan: the second report of the Tokai peritoneal dialysis registry. Clin Exp Nephrol, 2016.
- Nagata T, Sobajima H, Ohashi N, Hirakawa A, Katsuno T, Yasuda Y, Matsuo S, Tsuboi N, Maruyama S. Association between 24h Urinary Sodium and Potassium Excretion and Estimated Glomerular Filtration Rate (eGFR) Decline or Death in Patients with Diabetes Mellitus and eGFR More than 30 ml/min/1.73m2. PLoS One, 2016; 11: e0152306.
- Sawai A, Yasuda Y, Suzuki S, Ishii H, Goto M, Kato S, Hayashi M, Maruyama S, Murohara T, Oiso Y, Matsuo S. Impact of non-invasive cardiovascular screening programs as a predictor of cardiovascular events among asymptomatic chronic kidney disease patients. Clin Exp Nephrol, 2016; 20: 416-424.
- Takayama Y, Yasuda Y, Suzuki S, Shibata Y, Tatami Y, Shibata K, Niwa M, Sawai A, Morimoto R, Kato S, Ishii H, Maruyama S, Murohara T. Relationship between abdominal aortic and coronary artery calcification as detected by computed tomography in chronic kidney disease patients. Heart Vessels, 2016; 31: 1030-1037.
- Tawada M, Ito Y, Hamada C, Honda K, Mizuno M, Suzuki Y, Sakata F, Terabayashi T, Matsukawa Y, Maruyama S, Imai E, Matsuo S, Takei Y. Vascular Endothelial Cell Injury Is an Important Factor in the Development of Encapsulating Peritoneal Sclerosis in Long-Term Peritoneal Dialysis Patients. PLoS One, 2016; 11: e0154644.
- Asano S, Mizuno S, Okachi S, Aso H, Wakahara K, Hashimoto N, Ito S, Kozaki Y, Katsuno T, Maruyama S, Hasegawa Y. Antineutrophil Cytoplasmic Antibody-associated Vasculitis Superimposed on Infection-related Glomerulonephritis Secondary to Pulmonary Mycobacterium avium Complex Infection. Intern Med, 2016; 55: 2439-2445.
- Endo N, Tsuboi N, Furuhashi K, Shi Y, Du Q, Abe T, Hori M, Imaizumi T, Kim H, Katsuno T, Ozaki T, Kosugi T, Matsuo S, Maruyama S. Urinary soluble CD163 level reflects glomerular inflammation in human lupus nephritis. Nephrol Dial Transplant, 2016.
- Hamada M, Yasuda Y, Kato S, Arafuka H, Goto M, Hayashi M, Kajita E, Maruyama S. The effectiveness and safety of modest exercise in Japanese patients with chronic kidney disease: a single-armed interventional study. Clin Exp Nephrol, 2016; 20: 204-211.
- Hattori M, Iwano M, Sako M, Honda M, Okada H, Akioka Y, Ashida A, Kawasaki Y, Kiyomoto H, Terada Y, Hirano D, Fujieda M, Fujimoto S, Masaki T, Maruyama S, Mastuo S. Transition of adolescent and young adult patients with childhood-onset chronic kidney disease from pediatric to adult renal services: a nationwide survey in Japan. Clin Exp Nephrol, 2016.
- Hayashi H, Sato W, Kosugi T, Nishimura K, Sugiyama D, Asano N, Ikematsu S, Komori K, Nishiwaki K, Kadomatsu K, Matsuo S, Maruyama S, Yuzawa Y. Efficacy of urinary midkine as a biomarker in patients with acute kidney injury. Clin Exp Nephrol, 2016.
- Hishida M, Tamai H, Morinaga T, Maekawa M, Aoki T, Tomida H, Komatsu S, Kamiya T, Maruyama S, Matsuo S, Inaguma D. Aichi cohort study of the prognosis in patients newly initiated into dialysis (AICOPP): baseline characteristics and trends observed in diabetic nephropathy. Clin Exp Nephrol, 2016; 20: 795-807.
- Imai E, Maruyama S, Nangaku M, Hirakata H, Hayashi T, Narita I, Kono H, Nakatani E, Morita S, Tsubakihara Y, Akizawa T. Rationale and study design of a randomized controlled trial to assess the effects of maintaining hemoglobin levels using darbepoetin alfa on prevention of development of end-stage kidney disease in non-diabetic CKD patients (PREDICT Trial). Clin Exp Nephrol, 2016; 20: 71-76.
- Imaizumi T, Ando M, Nakatochi M, Maruyama S, Yasuda Y, Honda H, Kuwatsuka Y, Kato S, Kondo T, Iwata M, Nakashima T, Yasui H, Takamatsu H, Okajima H, Yoshida Y, Matsuo S. Association of interactions between dietary salt consumption and hypertension-susceptibility genetic polymorphisms with blood pressure among Japanese male workers. Clin Exp Nephrol, 2016.
- Imaizumi T, Ando M, Nakatochi M, Yasuda Y, Honda H, Kuwatsuka Y, Kato S, Kondo T, Iwata M, Nakashima T, Yasui H, Takamatsu H, Okajima H, Yoshida Y, Maruyama S. Effect of dietary energy and polymorphisms in BRAP and GHRL on obesity and metabolic traits. Obes Res Clin Pract, 2016.
- Imaizumi T, Nakatochi M, Akiyama S, Yamaguchi M, Kurosawa H, Hirayama Y, Katsuno T, Tsuboi N, Hara M, Maruyama S. Urinary Podocalyxin as a Biomarker to Diagnose Membranous Nephropathy. PLoS One, 2016; 11: e0163507.
- 2015
- Yokoyama H, Sugiyama H, Narita I, Saito T, Yamagata K, Nishio S, Fujimoto S, Mori N, Yuzawa Y, Okuda S, Maruyama S, Sato H, Ueda Y, Makino H, Matsuo S. Outcomes of primary nephrotic syndrome in elderly Japanese: retrospective analysis of the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol, 2015; 19: 496-505.
- Yamaguchi M, Ando M, Kato S, Katsuno T, Kato N, Kosugi T, Sato W, Tsuboi N, Yasuda Y, Mizuno M, Ito Y, Matsuo S, Maruyama S. Increase of Antimyeloperoxidase Antineutrophil Cytoplasmic Antibody (ANCA) in Patients with Renal ANCA-associated Vasculitis: Association with Risk to Relapse. J Rheumatol, 2015; 42: 1853-1860.
- Terabayashi T, Ito Y, Mizuno M, Suzuki Y, Kinashi H, Sakata F, Tomita T, Iguchi D, Tawada M, Nishio R, Maruyama S, Imai E, Matsuo S, Takei Y. Vascular endothelial growth factor receptor-3 is a novel target to improve net ultrafiltration in methylglyoxal-induced peritoneal injury. Lab Invest, 2015; 95: 1029-1043.
- Tatami Y, Yasuda Y, Suzuki S, Ishii H, Sawai A, Shibata Y, Ota T, Shibata K, Niwa M, Morimoto R, Hayashi M, Kato S, Maruyama S, Murohara T. Impact of abdominal aortic calcification on long-term cardiovascular outcomes in patients with chronic kidney disease. Atherosclerosis, 2015; 243: 349-355.
- Shimbo Y, Suzuki S, Ishii H, Shibata Y, Tatami Y, Harata S, Osugi N, Ota T, Tanaka A, Shibata K, Mizukoshi T, Yasuda Y, Maruyama S, Murohara T. Association of Estimated Glomerular Filtration Rate and Proteinuria With Lipid-Rich Plaque in Coronary Artery Disease. Circ J, 2015; 79: 2263-2270.
- Shibata K, Yasuda Y, Kobayashi R, Ando Y, Shimokata T, Kamiya H, Hayashi M, Maruyama S, Matsuo S, Nakao M, Tsuchiya T, Teramachi H. Renal function evaluation in patients with cancer who were scheduled to receive carboplatin or S-1. Clin Exp Nephrol, 2015; 19: 1107-1113.
- Sei Y, Mizuno M, Suzuki Y, Imai M, Higashide K, Harris CL, Sakata F, Iguchi D, Fujiwara M, Kodera Y, Maruyama S, Matsuo S, Ito Y. Expression of membrane complement regulators, CD46, CD55 and CD59, in mesothelial cells of patients on peritoneal dialysis therapy. Mol Immunol, 2015; 65: 302-309.
- Sato Y, Sato W, Maruyama S, Wilcox CS, Falck JR, Masuda T, Kosugi T, Kojima H, Maeda K, Furuhashi K, Ando M, Imai E, Matsuo S, Kadomatsu K. Midkine Regulates BP through Cytochrome P450-Derived Eicosanoids. J Am Soc Nephrol, 2015; 26: 1806-1815.
- Saka Y, Ito Y, Iida Y, Maruyama S, Matsuo S. Efficacy and safety of fluoroscopic manipulation using the alpha-replacer for peritoneal catheter malposition. Clin Exp Nephrol, 2015; 19: 521-526.
- Nakatochi M, Ushida Y, Yasuda Y, Yoshida Y, Kawai S, Kato R, Nakashima T, Iwata M, Kuwatsuka Y, Ando M, Hamajima N, Kondo T, Oda H, Hayashi M, Kato S, Yamaguchi M, Maruyama S, Matsuo S, Honda H. Identification of an interaction between VWF rs7965413 and platelet count as a novel risk marker for metabolic syndrome: an extensive search of candidate polymorphisms in a case-control study. PLoS One, 2015; 10: e0117591.
- Nagata T, Yasuda Y, Ando M, Abe T, Katsuno T, Kato S, Tsuboi N, Matsuo S, Maruyama S. Clinical impact of kidney function on presepsin levels. PLoS One, 2015; 10: e0129159.
- Maeda K, Kosugi T, Sato W, Kojima H, Sato Y, Kamimura D, Kato N, Tsuboi N, Yuzawa Y, Matsuo S, Murakami M, Maruyama S, Kadomatsu K. CD147/basigin limits lupus nephritis and Th17 cell differentiation in mice by inhibiting the interleukin-6/STAT-3 pathway. Arthritis Rheumatol, 2015; 67: 2185-2195.
- Kosugi T, Maeda K, Sato W, Maruyama S, Kadomatsu K. CD147 (EMMPRIN/Basigin) in kidney diseases: from an inflammation and immune system viewpoint. Nephrol Dial Transplant, 2015; 30: 1097-1103.
- Kato S, Maruyama S, Makino H, Wada J, Ogawa D, Uzu T, Araki H, Koya D, Kanasaki K, Oiso Y, Goto M, Nishiyama A, Kobori H, Imai E, Ando M, Matsuo S. Anti-albuminuric effects of spironolactone in patients with type 2 diabetic nephropathy: a multicenter, randomized clinical trial. Clin Exp Nephrol, 2015; 19: 1098-1106.
- Hayashi N, Akiyama S, Okuyama H, Matsui Y, Adachi H, Yamaya H, Maruyama S, Imai E, Matsuo S, Yokoyama H. Clinicopathological characteristics of M-type phospholipase A2 receptor (PLA2R)-related membranous nephropathy in Japanese. Clin Exp Nephrol, 2015; 19: 797-803.
- Hattori Y, Kim H, Tsuboi N, Yamamoto A, Akiyama S, Shi Y, Katsuno T, Kosugi T, Ueda M, Matsuo S, Maruyama S. Therapeutic Potential of Stem Cells from Human Exfoliated Deciduous Teeth in Models of Acute Kidney Injury. PLoS One, 2015; 10: e0140121.
- Baba M, Shimbo T, Horio M, Ando M, Yasuda Y, Komatsu Y, Masuda K, Matsuo S, Maruyama S. Longitudinal Study of the Decline in Renal Function in Healthy Subjects. PLoS One, 2015; 10: e0129036.
- Akiyama S, Akiyama M, Imai E, Ozaki T, Matsuo S, Maruyama S. Prevalence of anti-phospholipase A2 receptor antibodies in Japanese patients with membranous nephropathy. Clin Exp Nephrol, 2015; 19: 653-660.
- Abe T, Kato S, Tsuruta Y, Sugiura S, Katsuno T, Kosugi T, Tsuboi N, Matsuo S, Maruyama S. Neutrophil/lymphocyte ratio as a predictor of cardiovascular events in incident dialysis patients: a Japanese prospective cohort study. Clin Exp Nephrol, 2015; 19: 718-724.
- 2014
- Yamaguchi M, Yoshioka T, Yamakawa T, Maeda M, Shimizu H, Fujita Y, Maruyama S, Ito Y, Matsuo S. Anti-neutrophil cytoplasmic antibody-associated vasculitis associated with infectious mononucleosis due to primary Epstein-Barr virus infection: report of three cases. Clin Kidney J, 2014; 7: 45-48.
- Yamaguchi M, Ando M, Yamamoto R, Akiyama S, Kato S, Katsuno T, Kosugi T, Sato W, Tsuboi N, Yasuda Y, Mizuno M, Ito Y, Matsuo S, Maruyama S. Smoking is a risk factor for the progression of idiopathic membranous nephropathy. PLoS One, 2014; 9: e100835.
- Yamaguchi M, Ando M, Yamamoto R, Akiyama S, Kato S, Katsuno T, Kosugi T, Sato W, Tsuboi N, Yasuda Y, Mizuno M, Ito Y, Matsuo S, Maruyama S. Patient age and the prognosis of idiopathic membranous nephropathy. PLoS One, 2014; 9: e110376.
- Wada T, Nangaku M, Maruyama S, Imai E, Shoji K, Kato S, Endo T, Muso E, Kamata K, Yokoyama H, Fujimoto K, Obata Y, Nishino T, Kato H, Uchida S, Sasatomi Y, Saito T, Matsuo S. A multicenter cross-sectional study of circulating soluble urokinase receptor in Japanese patients with glomerular disease. Kidney Int, 2014; 85: 641-648.
- Tsuboi N, Maruyama S, Matsuo S, Imai E. A ray of light in the dark: alternative approaches to the assessment and treatment of ischemic nephropathy. Nephrol Dial Transplant, 2014; 29: 228-231.
- Takahashi H, Ito Y, Ishii H, Aoyama T, Kamoi D, Kasuga H, Yasuda K, Maruyama S, Matsuo S, Murohara T, Yuzawa Y. Geriatric nutritional risk index accurately predicts cardiovascular mortality in incident hemodialysis patients. J Cardiol, 2014; 64: 32-36.
- Shinjo H, Sato W, Imai E, Kosugi T, Hayashi H, Nishimura K, Nishiwaki K, Yuzawa Y, Matsuo S, Maruyama S. Comparison of kidney disease: improving global outcomes and acute kidney injury network criteria for assessing patients in intensive care units. Clin Exp Nephrol, 2014; 18: 737-745.
- Shi Y, Tsuboi N, Furuhashi K, Du Q, Horinouchi A, Maeda K, Kosugi T, Matsuo S, Maruyama S. Pristane-induced granulocyte recruitment promotes phenotypic conversion of macrophages and protects against diffuse pulmonary hemorrhage in Mac-1 deficiency. J Immunol, 2014; 193: 5129-5139.
- Nagaya H, Kosugi T, Maeda-Hori M, Maeda K, Sato Y, Kojima H, Hayashi H, Kato N, Ishimoto T, Sato W, Yuzawa Y, Matsuo S, Kadomatsu K, Maruyama S. CD147/basigin reflects renal dysfunction in patients with acute kidney injury. Clin Exp Nephrol, 2014; 18: 746-754.
- Miyashita H, Chikazawa M, Otaki N, Hioki Y, Shimozu Y, Nakashima F, Shibata T, Hagihara Y, Maruyama S, Matsumi N, Uchida K. Lysine pyrrolation is a naturally-occurring covalent modification involved in the production of DNA mimic proteins. Sci Rep, 2014; 4: 5343.
- Maeda-Hori M, Kosugi T, Kojima H, Sato W, Inaba S, Maeda K, Nagaya H, Sato Y, Ishimoto T, Ozaki T, Tsuboi N, Muro Y, Yuzawa Y, Imai E, Johnson RJ, Matsuo S, Kadomatsu K, Maruyama S. Plasma CD147 reflects histological features in patients with lupus nephritis. Lupus, 2014; 23: 342-352.
- Kim H, Mizuno M, Furuhashi K, Katsuno T, Ozaki T, Yasuda K, Tsuboi N, Sato W, Suzuki Y, Matsuo S, Ito Y, Maruyama S. Rat adipose tissue-derived stem cells attenuate peritoneal injuries in rat zymosan-induced peritonitis accompanied by complement activation. Cytotherapy, 2014; 16: 357-368.
- Ito Y, Mizuno M, Suzuki Y, Tamai H, Hiramatsu T, Ohashi H, Ito I, Kasuga H, Horie M, Maruyama S, Yuzawa Y, Matsubara T, Matsuo S, Nagoya Spiro Study G. Long-term effects of spironolactone in peritoneal dialysis patients. J Am Soc Nephrol, 2014; 25: 1094-1102.
- 2013
- Yamamoto J, Sato W, Kosugi T, Yamamoto T, Kimura T, Taniguchi S, Kojima H, Maruyama S, Imai E, Matsuo S, Yuzawa Y, Niki I. Distribution of hydrogen sulfide (H(2)S)-producing enzymes and the roles of the H(2)S donor sodium hydrosulfide in diabetic nephropathy. Clin Exp Nephrol, 2013; 17: 32-40.
- Mizuno T, Mizuno M, Imai M, Suzuki Y, Kushida M, Noda Y, Maruyama S, Okada H, Okada N, Matsuo S, Ito Y. Anti-C5a complementary peptide ameliorates acute peritoneal injury induced by neutralization of Crry and CD59. Am J Physiol Renal Physiol, 2013; 305: F1603-1616.
- Mizuno M, Suzuki Y, Nonaka K, Sei Y, Maruyama S, Matsuo S, Ito Y. Perforative peritonitis caused by appendicitis in a patient on peritoneal dialysis. Intern Med, 2013; 52: 1177-1181.
- Maruyama S. [Progressive renal diseases: recent advances in diagnosis and treatments. Topics: I. Diagnosis; 4. Nephrotic syndrome]. Nihon Naika Gakkai Zasshi, 2013; 102: 1098-1104.
- Kojima H, Kosugi T, Sato W, Sato Y, Maeda K, Kato N, Kato K, Inaba S, Ishimoto T, Tsuboi N, Matsuo S, Maruyama S, Yuzawa Y, Kadomatsu K. Deficiency of growth factor midkine exacerbates necrotizing glomerular injuries in progressive glomerulonephritis. Am J Pathol, 2013; 182: 410-419.
- Katsuno T, Ozaki T, Saka Y, Furuhashi K, Kim H, Yasuda K, Yamamoto T, Sato W, Tsuboi N, Mizuno M, Ito Y, Imai E, Matsuo S, Maruyama S. Low serum cultured adipose tissue-derived stromal cells ameliorate acute kidney injury in rats. Cell Transplant, 2013; 22: 287-297.
- Furuhashi K, Tsuboi N, Shimizu A, Katsuno T, Kim H, Saka Y, Ozaki T, Sado Y, Imai E, Matsuo S, Maruyama S. Serum-starved adipose-derived stromal cells ameliorate crescentic GN by promoting immunoregulatory macrophages. J Am Soc Nephrol, 2013; 24: 587-603.
- Chikazawa M, Otaki N, Shibata T, Miyashita H, Kawai Y, Maruyama S, Toyokuni S, Kitaura Y, Matsuda T, Uchida K. Multispecificity of immunoglobulin M antibodies raised against advanced glycation end products: involvement of electronegative potential of antigens. J Biol Chem, 2013; 288: 13204-13214.
- 2012
- Yasuda K, Ozaki T, Saka Y, Yamamoto T, Gotoh M, Ito Y, Yuzawa Y, Matsuo S, Maruyama S. Autologous cell therapy for cisplatin-induced acute kidney injury by using non-expanded adipose tissue-derived cells. Cytotherapy, 2012; 14: 1089-1100.
- Toda S, Ito Y, Mizuno M, Suzuki Y, Ito I, Hiramatsu H, Ozaki T, Tsuboi N, Sato W, Maruyama S, Imai E, Matsuo S. Asymptomatic diverticulosis identified by computed tomography is not a risk factor for enteric peritonitis. Nephrol Dial Transplant, 2012; 27: 2511-2516.
- Tatematsu M, Yasuda Y, Morita Y, Sakamoto I, Kurata K, Naruse T, Yamamoto R, Tsuboi N, Sato W, Imai E, Matsuo S, Maruyama S. Complete remission within 2 years predicts a good prognosis after methylprednisolone pulse therapy in patients with IgA nephropathy. Clin Exp Nephrol, 2012; 16: 883-891.
- Takahashi R, Ito Y, Takahashi H, Ishii H, Kasuga H, Mizuno M, Suzuki Y, Yuzawa Y, Maruyama S, Murohara T, Imai E, Matsuo S. Combined values of serum albumin, C-reactive protein and body mass index at dialysis initiation accurately predicts long-term mortality. Am J Nephrol, 2012; 36: 136-143.
- Suzuki Y, Ito Y, Mizuno M, Kinashi H, Sawai A, Noda Y, Mizuno T, Shimizu H, Fujita Y, Matsui K, Maruyama S, Imai E, Matsuo S, Takei Y. Transforming growth factor-beta induces vascular endothelial growth factor-C expression leading to lymphangiogenesis in rat unilateral ureteral obstruction. Kidney Int, 2012; 81: 865-879.
- Okada R, Yasuda Y, Tsushita K, Wakai K, Hamajima N, Matsuo S. Glomerular hyperfiltration in prediabetes and prehypertension. Nephrol Dial Transplant, 2012; 27: 1821-1825.
- Nishiwaki S, Nakayama T, Saito S, Mizuno H, Ozaki T, Takahashi Y, Maruyama S, Nishida T, Murata M, Kojima S, Naoe T. Efficacy and safety of human adipose tissue-derived mesenchymal stem cells for supporting hematopoiesis. Int J Hematol, 2012; 96: 295-300.
- Kato S, Lindholm B, Stenvinkel P, Ekstrom TJ, Luttropp K, Yuzawa Y, Yasuda Y, Tsuruta Y, Maruyama S. DNA hypermethylation and inflammatory markers in incident Japanese dialysis patients. Nephron Extra, 2012; 2: 159-168.
- Kato H, Mizuno T, Mizuno M, Sawai A, Suzuki Y, Kinashi H, Nagura F, Maruyama S, Noda Y, Yamada K, Matsuo S, Ito Y. Atrial natriuretic peptide ameliorates peritoneal fibrosis in rat peritonitis model. Nephrol Dial Transplant, 2012; 27: 526-536.
- Ito I, Ito Y, Mizuno M, Suzuki Y, Yasuda K, Ozaki T, Kosugi T, Yasuda Y, Sato W, Tsuboi N, Maruyama S, Imai E, Matsuo S. A rare case of acute kidney injury associated with autoimmune hemolytic anemia and thrombocytopenia after long-term usage of oxaliplatin. Clin Exp Nephrol, 2012; 16: 490-494.
- Ishii H, Toriyama T, Aoyama T, Takahashi H, Tanaka M, Yoshikawa D, Hayashi M, Yasuda Y, Maruyama S, Matsuo S, Matsubara T, Murohara T. Percutaneous coronary intervention with bare metal stent vs. drug-eluting stent in hemodialysis patients. Circ J, 2012; 76: 1609-1615.
- Ishii H, Kumada Y, Takahashi H, Toriyama T, Aoyama T, Tanaka M, Yoshikawa D, Hayashi M, Kasuga H, Yasuda Y, Maruyama S, Matsubara T, Matsuo S, Murohara T. Impact of diabetes and glycaemic control on peripheral artery disease in Japanese patients with end-stage renal disease: long-term follow-up study from the beginning of haemodialysis. Diabetologia, 2012; 55: 1304-1309.
- Inaba S, Nagahara S, Makita N, Tarumi Y, Ishimoto T, Matsuo S, Kadomatsu K, Takei Y. Atelocollagen-mediated systemic delivery prevents immunostimulatory adverse effects of siRNA in mammals. Mol Ther, 2012; 20: 356-366.
- 2011
- Watanabe T, Maruyama S, Yamamoto T, Kamo I, Yasuda K, Saka Y, Ozaki T, Yuzawa Y, Matsuo S, Gotoh M. Increased urethral resistance by periurethral injection of low serum cultured adipose-derived mesenchymal stromal cells in rats. Int J Urol, 2011; 18: 659-666.
- Suzuki Y, Mizuno M, Nakashima R, Hiramatsu H, Toda S, Sato W, Tsuboi N, Ito I, Maruyama S, Imai E, Matsuo S, Ito Y. A case of perforative peritonitis caused by a piece of bamboo in a patient on peritoneal dialysis. Clin Exp Nephrol, 2011; 15: 962-965.
- Sawai A, Ito Y, Mizuno M, Suzuki Y, Toda S, Ito I, Hattori R, Matsukawa Y, Gotoh M, Takei Y, Yuzawa Y, Matsuo S. Peritoneal macrophage infiltration is correlated with baseline peritoneal solute transport rate in peritoneal dialysis patients. Nephrol Dial Transplant, 2011; 26: 2322-2332.
- Saka Y, Furuhashi K, Katsuno T, Kim H, Ozaki T, Iwasaki K, Haneda M, Sato W, Tsuboi N, Ito Y, Matsuo S, Kobayashi T, Maruyama S. Adipose-derived stromal cells cultured in a low-serum medium, but not bone marrow-derived stromal cells, impede xenoantibody production. Xenotransplantation, 2011; 18: 196-208.
- Saito S, Murakumo Y, Tsuzuki T, Dambara A, Kato T, Enomoto A, Asai N, Maruyama S, Matsuo S, Takahashi M. Analysis of glial cell line-derived neurotrophic factor-inducible zinc finger protein 1 expression in human diseased kidney. Hum Pathol, 2011; 42: 848-858.
- Mizuno T, Mizuno M, Morgan BP, Noda Y, Yamada K, Okada N, Yuzawa Y, Matsuo S, Ito Y. Specific collaboration between rat membrane complement regulators Crry and CD59 protects peritoneum from damage by autologous complement activation. Nephrol Dial Transplant, 2011; 26: 1821-1830.
- Mizuno M, Ito Y, Tanaka A, Suzuki Y, Hiramatsu H, Watanabe M, Tsuruta Y, Matsuoka T, Ito I, Tamai H, Kasuga H, Shimizu H, Kurata H, Inaguma D, Hiramatsu T, Horie M, Naruse T, Maruyama S, Imai E, Yuzawa Y, Matsuo S. Peritonitis is still an important factor for withdrawal from peritoneal dialysis therapy in the Tokai area of Japan. Clin Exp Nephrol, 2011; 15: 727-737.
- Mizuno M, Ito Y, Masuda T, Toda S, Hiramatsu H, Suzuki Y, Ozaki T, Yasuda Y, Ito I, Tsuboi N, Sato W, Maruyama S, Imai E, Matsuo S. A case of fulminant peritonitis caused by Streptococcus mitis in a patient on peritoneal dialysis. Intern Med, 2011; 50: 471-474.
- Mizuno M, Ito Y, Hayasaki T, Suzuki Y, Hiramatsu H, Toda S, Mizuno T, Tatematsu M, Ozaki T, Yasuda Y, Sato W, Tsuboi N, Ito I, Maruyama S, Imai E, Matsuo S. A case of acute renal failure caused by cholesterol embolization after carotid artery stenting that was improved by peritoneal dialysis. Intern Med, 2011; 50: 1719-1723.
- Kato N, Kosugi T, Sato W, Ishimoto T, Kojima H, Sato Y, Sakamoto K, Maruyama S, Yuzawa Y, Matsuo S, Kadomatsu K. Basigin/CD147 promotes renal fibrosis after unilateral ureteral obstruction. Am J Pathol, 2011; 178: 572-579.
- Kato K, Kosugi T, Sato W, Arata-Kawai H, Ozaki T, Tsuboi N, Ito I, Tawada H, Yuzawa Y, Matsuo S, Kadomatsu K, Maruyama S. Growth factor Midkine is involved in the pathogenesis of renal injury induced by protein overload containing endotoxin. Clin Exp Nephrol, 2011; 15: 346-354.
- Imai E, Yasuda Y, Horio M, Shibata K, Kato S, Mizutani Y, Imai J, Hayashi M, Kamiya H, Oiso Y, Murohara T, Maruyama S, Matsuo S. Validation of the equations for estimating daily sodium excretion from spot urine in patients with chronic kidney disease. Clin Exp Nephrol, 2011; 15: 861-867.