Laboratories
- Back
- Top > Laboratories > Clinical Neurosciences > Neurosurgery/Frontier Surgical Neuroscience/Endovascular Neurosurgery
Clinical NeurosciencesNeurosurgery/Frontier Surgical Neuroscience/Endovascular Neurosurgery
Introduction
Neurosurgical operations:
Nagoya University Department of Neurosurgery boasts a fully equipped and highly precise robotic-assisted "Neuronavigation" surgical support system, including intraoperative MRI, navigation system, Neuromate, etc. Moreover, intraoperative neuro-monitoring and awake surgeries add to the safety and have achieved better results with functional preservation even in the most complicated neurosurgical cases.
Development of cutting edge medicine for brain tumors:
Microcapsule embedded interferon-β gene therapy for malignant brain tumors was started, in our department in April 2000, as a clinical research of advanced medicine. We are preparing for the world`s first clinical study of brain tumor nucleic acid medicine.
Cell therapy and Neuro-regeneration:
With the pivotal role of "Advanced Medicine and Clinical Research Support Centre" (formerly Genetic and Nerve Regeneration Centre) of Nagoya University, we are preparing for a cell and tissue preparation center (ISO9001:2008, ISO13485:2003 certified) best suited to "clinical research" and "doctor-led clinical study." Clinical study of dendritic cell therapy, by sensitizing brain tumor specific antigen expression, for malignant brain tumors is undergoing at this Centre, with the cooperation from the blood transfusion department of Nagoya University Hospital and Pittsburgh University.
Comprehensive genomic analysis of brain tumors:
As a result of our work on genomic analysis, identification of novel prognostic factors and application to tailor made therapy has been made possible. We are also developing novel molecular target therapy by identifying new target molecules in brain tumors.
Research Projects
1. Mutational landscape and clonal architecture in grade-II and III gliomas. : Project leader: Atsushi NATSUME, MD, PhD
Key Points
1. Over 700 samples of grade II or III gliomas were analyzed by next-generation sequencer.
2. Regardless of histology types, LGGs are grouped into three distinct subgroups (Type I, II, and III tumors) with different clinical/biological behaviors, according to sets of genetic lesions characteristic to each subtype.
3. Major driver alterations showed strong positive and negative correlations with each other and temporal orders to occur, suggesting strong functional interplay between these mutations, which were also supported explicit serial/multi-regional sampling analysis.
4. Heterogeneity within a tumor and between tumors at different time points was prominent in grade II and III gliomas. Nevertheless, common occurrence of parallel mutations found in TP53/ATRX, CIC, FUBP1 genes indicated central roles of these mutations in glioma development.
5. Multi-regional sampling delineated how grade II and III glioma originated and propagated to generate extensive intratumor heterogeneity through acquiring new mutations in a complex but still ordered fashion.
Summary
Dr. Atsushi Natsume, Department of neurosurgery, Nagoya University Graduate School of Medicine (Dean: Masahide Takahashi, M.D., Ph.D.), and colleagues elucidated Mutational landscape and clonal architecture in grade-II and III gliomas. This study was reported online April 13th, 2015 in Nature Genetics.
Grade II/III gliomas account for approximately one third of all gliomas. Although grade II/III gliomas are typically slowly progressive, their clinical course is invariably indolent and most patients ultimately succumb to death. In contrast to glioblastoma (GBM), our knowledge about the genetic lesions and clonal evolution in grade II/III gliomas is still incomplete.
Main findings are as follow;
1. Over 700 samples of grade II or III gliomas were analyzed by next-generation sequencer.
2. Regardless of histology types, LGGs are grouped into three distinct subgroups (Type I, II, and III tumors) with different clinical/biological behaviors, according to sets of genetic lesions characteristic to each subtype.
3. Major driver alterations showed strong positive and negative correlations with each other and temporal orders to occur, suggesting strong functional interplay between these mutations, which were also supported explicit serial/multi-regional sampling analysis,
4. Heterogeneity within a tumor and between tumors at different time points was prominent in grade II and III gliomas. Nevertheless, common occurrence of parallel mutations found in TP53/ATRX, CIC, FUBP1 genes indicated central roles of these mutations in glioma development,
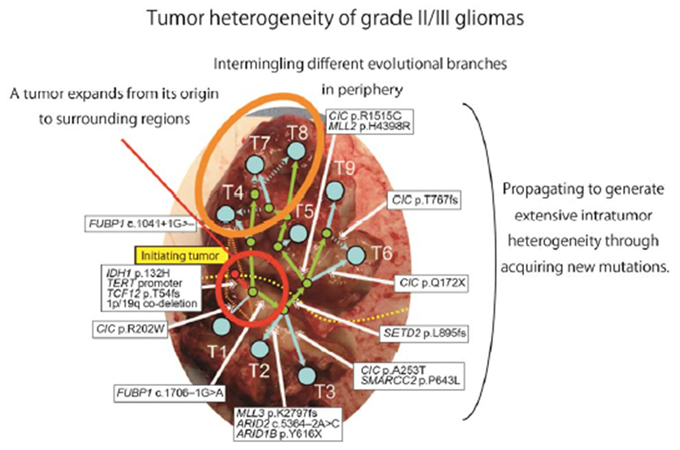
5. Multi-regional sampling delineated how grade II and III glioma originated and propagated to generate extensive intratumor heterogeneity through acquiring new mutations in a complex but still ordered fashion.
Research Background
Grade II/III gliomas account for approximately one third of all gliomas. Although grade II/III gliomas are typically slowly progressive, their clinical course is invariably indolent and most patients ultimately succumb to death. In contrast to glioblastoma (GBM), our knowledge about the genetic lesions and clonal evolution in grade II/III gliomas is still incomplete.
Dr. Atsushi Natsume, Department of neurosurgery, Nagoya University Graduate School of Medicine (Dean: Masahide Takahashi, M.D., Ph.D.), and colleagues analyzed over 700 grade II/III gliomas and revealed mutational landscape and clonal architecture.
Research Results
Including large data of whole exome/targeted sequencing and copy number analysis in 757 grade II/III glioma cases from combined Japanese (N = 332) and TCGA (N = 425) cohorts, this represents the largest genetic study ever performed for grade II/III gliomas, revealing an entire picture of grade II/III gliomas. Massive parallel sequencing revealed grade II/III gliomas were clearly grouped into three subgroups with or without IDH1/2 mutation and 1p/19q co-deletion (Figure 1).
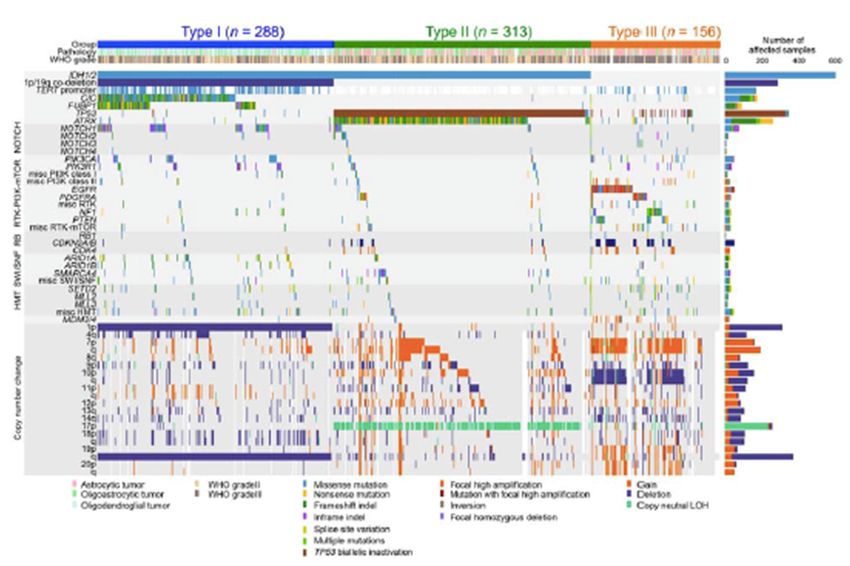
Mutations showed significant positive/negative correlations and chronological hierarchy as inferred from different allelic burdens among coexisting mutations (Figure2). All mutations in IDH1 and TERT promoter as well as 1p/19q co-deletion in Type-I tumors and most TP53 in Type-II tumors were found as early event. Multi-/serial sampling analyses supposed these mutational orders.
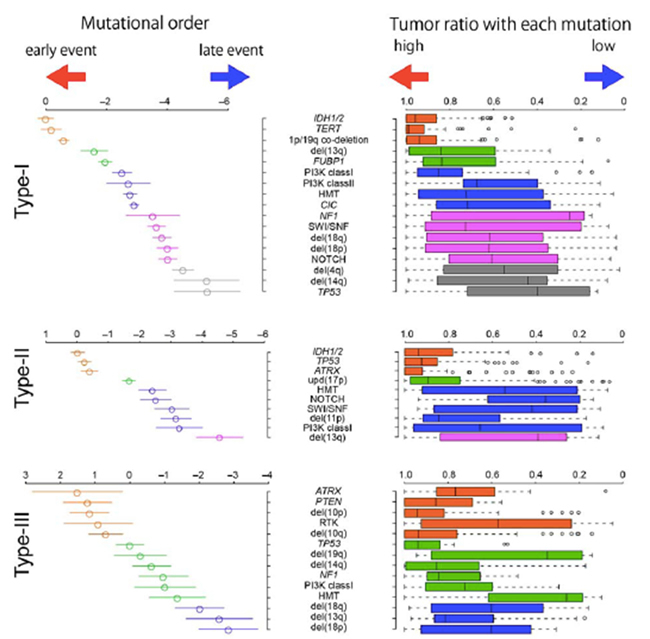
Extensive serial/multi-regional sampling analyses further revealed high degrees of temporal/spatial heterogeneity generated during tumor expansion and relapse. Figure 3 is representative case.
Research Summary and Future Perspective
These finding provided the basic information of grade II/III glioma pathogenesis and will lead to the development of new therapy for grade II/III gliomas.
The authors and title of the paper
Hiromichi Suzuki, Kosuke Aoki, Kenichi Chiba, Yusuke Sato, Yusuke Shiozawa, Yuichi
Shiraishi, Teppei Shimamura, Atsushi Niida, Kazuya Motomura, Fumiharu Ohka, Takashi
Yamamoto, Kuniaki Tanahashi, Melissa Ranjit, Toshihiko Wakabayashi, Tetsuichi Yoshizato,
Keisuke Kataoka, Kenichi Yoshida, Yasunobu Nagata, Aiko Sato-Otsubo, Hiroko Tanaka,
Masashi Sanada, Yutaka Kondo, Hideo Nakamura, Masahiro Mizoguchi, Tatsuya Abe,
Yoshihiro Muragaki, Reiko Watanabe, Ichiro Ito, Satoru Miyano, Atsushi Natsume and Seishi
Ogawa. Mutational landscape and clonal architecture in grade-II and III gliomas. Nature
Genetics, April 13, 2015.
2. CAR T cells targeting podoplanin reduce orthotopic glioblastoma in mouse brains : Project leader: Atsushi NATSUME, MD, PhD
Key Points
○We constructed a third generation CAR that targets PDPN and its successful lentivirus-mediated expression on human T cells.
○We showed that the generated CAR T cells were specific and effective against PDPN-positive GBM cells in vitro.
○Systemic injection of the generated T cells significantly increased survival time in vivo.
Summary
Glioblastoma (GBM) is the most common and lethal primary malignant brain tumor in adults with a 5-year overall survival rate of less than 10%. Novel therapies are required to improve patient survival. Chimeric antigen receptor (CAR) transduced T cells can recognize predefined tumor surface antigens independent of major histocompatibility complex (MHC) restriction, which is often downregulated in gliomas. Podoplanin (PDPN) is a type I transmembrane mucin-like glycoprotein, expressed in the lymphatic endothelium. It is overexpressed in several solid tumors such as squamous cell carcinoma, testicular seminoma, malignant mesothelioma, and brain tumors including GBM.
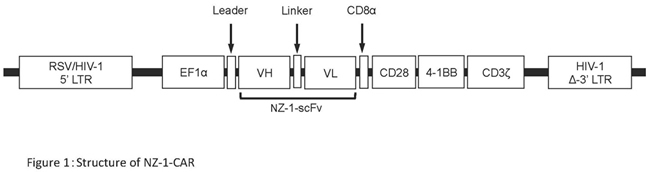
Dr. Atsushi Natsume, Department of neurosurgery, Nagoya University Graduate School of Medicine (Dean: Masahide Takahashi, M.D., Ph.D.), and colleagues generated a lentiviral vector expressing a third generation CAR comprising a PDPN-specific antibody [NZ-1-based single chain variable fragment (scFv)] with CD28, 4-1BB, and CD3ζ intracellular domains. CAR-transduced T cells were immunologically evaluated by calcein-mediated cytotoxic assay, ELISA, tumor size, and overall survival. The generated CAR T cells were specific and effective against PDPN-positive GBM cells in vitro. Systemic injection of the CAR T cells into an immunodeficient mouse model inhibited the growth of intracranial glioma xenografts and significantly increased survival time in vivo.
CAR T cell therapy that targets PDPN would be a promising adoptive immunotherapy to treat GBM.
Research Background
Glioblastoma (GBM) is the most common and lethal primary malignant brain tumor in adults with a 5-year overall survival rate of less than 10%. Novel therapies are required to improve patient survival.
In recent years, immunotherapy has emerged as a promising strategy for the treatment of GBM. Chimeric antigen receptors (CARs) were recombinant receptors that consisting of an extracellular domain derived from a single-chain variable fragment (scFv) taken from a tumor antigen-specific monoclonal antibody (mAb), a transmembrane domain, and a cytoplasmic signaling domain CD3 ζ chain (CD3ζ) derived from the T-cell receptor complex. CAR transduced T cells can recognize predefined tumor surface antigens independent of major histocompatibility complex (MHC) restriction, which is often downregulated in gliomas. Third generation CARs, combining two costimulatory domains such as CD28 and 4-1BB, have been described and are highly likely to lyse tumor cells.
We and other groups have generated several CARs against the antigens expressed in GBM, including epidermal growth factor receptor variant III (EGFRvIII), human epidermal growth factor receptor 2 (HER2), and interleukin-13 receptor alpha 2 (IL13Rα2).
Podoplanin (PDPN) is a type I transmembrane mucin-like glycoprotein expressed in the lymphatic endothelium. It is overexpressed in several solid tumors such as squamous cell carcinoma, testicular seminoma, malignant mesothelioma, and brain tumors including GBM. We previously produced a highly reactive mAb to PDPN , called NZ-1, and its recombinant scFv.
We generated a third generation of CAR that targeted PDPN, by using the NZ-1-based scFv. The generated CAR-transduced T cells were immunologically evaluated by calcein-mediated cytotoxic assay, ELISA, tumor size, and overall survival. The CAR T cells were specific and effective against PDPN-positive GBM cells in vitro. Systemic injection of the CAR T cells into an immunodeficient mouse model inhibited the growth of intracranial glioma xenografts and significantly increased survival time in vivo.
Research Results
We constructed a lentiviral vector tandem linked with the EF1α promoter followed by the leader sequence, NZ-1-based scFv, CD28, 4-1BB, and CD3ζ (Figure 1). The lentiviral vector was used to infect human T cells.
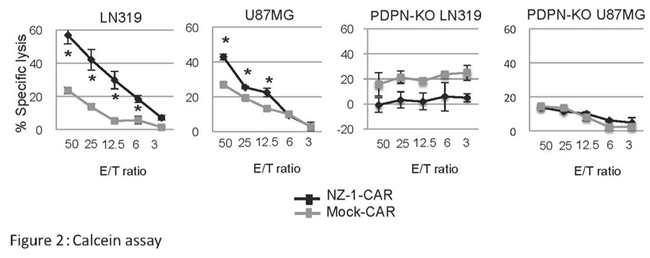
The calcein-based nonradioisotope cytotoxic assay indicated that PDPN-positive LN319 cells and U87MG cells were significantly lysed by NZ-1-CAR transduced T cells in an effector/target (E/T) ratio-dependent manner. In contrast, specific lysis was not observed against PDPN-KO LN319 and PDPN-KO U87MG cells (Figure 2).
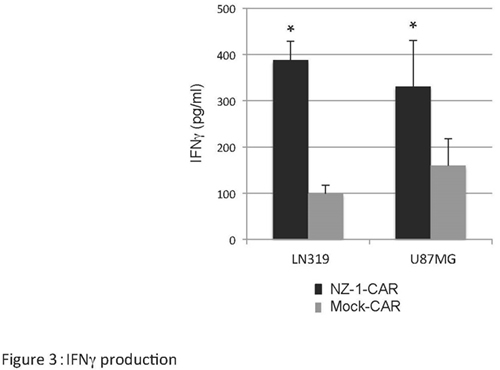
NZ-1-CAR transduced T cells coocultured with LN319 or U87MG cells released significantly much IFNγ than mock-transduced T cells (Figure 3). Thus, we successfully generated functional active NZ-1-CAR T cells that recognize PDPN.
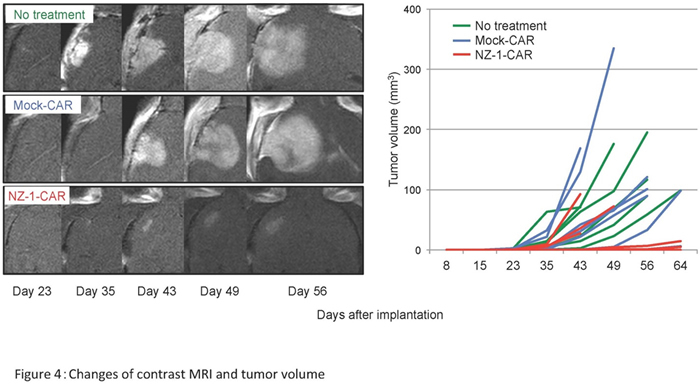
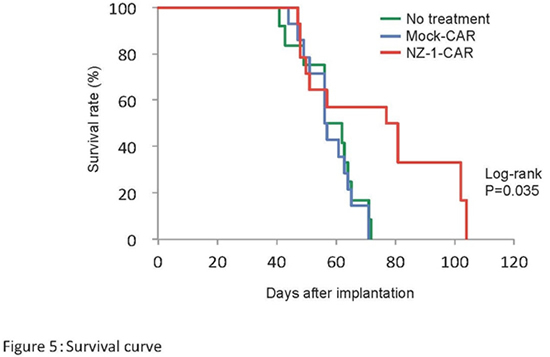
U87MG cells were stereotactically implanted into an immunodeficient mouse brain. Seven days after tumor implantation, NZ-1-CAR transduced T cells or mock-transduced T cells were infused intravenously via the tail vein. The non-treated mice were infused with PBS alone. The volume of gadolinium-enhanced tumors was evaluated by 3T-MRI sequentially. In approximately 60% of the mice treated with NZ-1-CAR T cells, the tumor grew markedly slower (Figure 4) and the mice survived significantly longer than that in the other two groups (Figure 5).
Research Summary and Future Perspective
CAR T cell therapy that targets PDPN would be a promising adoptive immunotherapy to treat GBM.
One of the concerns with PDPN-targeted CAR therapy is that PDPN is expressed in normal tissues, including the lymphatic endothelium, lung type I alveolar cells. We established a cancer-specific mAb (CasMab) to human PDPN. The CasMab can react with PDPN-expressing cancer cells, but not with normal cells such as lymphatic cells and type I alveolar cells. It may be useful to produce a new CAR using the CasMab for CAR therapy targeting PDPN.
Article
Satoshi Shiina, Masasuke Ohno, Fumiharu Ohka, Shunichiro Kuramitsu, Akane Yamamichi, Akira Kato, Kazuya Motomura, Kuniaki Tanahashi, Takashi Yamamoto, Reiko Watanabe, Ichiro Ito, Takeshi Senga, Michinari Hamaguchi, Toshihiko Wakabayashi, Mika K. Kaneko, Yukinari Kato, Vidyalakshmi Chandramohan, Darell D. Bigner, Atsushi Natsume. CAR T cells targeting podoplanin reduce orthotopic glioblastoma in mouse brains. Cancer Immunology Research ; Published OnlineFirst January 28, 2016.
3. An immuno-wall microdevice exhibits rapid and sensitive detection of IDH1-R132H mutation specific to grade II and III gliomas: Project leader: Atsushi NATSUME, MD, PhD
Key Points
○A micro-sized device “immuno-wall microdevice,” has been constructed, which can determine whether a sample is positive for the IDH1 mutation using only a small sample.
○This device features a chip with an attached highly-specific antibody, HMab-2, that binds to the protein produced by the gene in which the mutation has occurred.
○This novel approach takes only less than 15 minutes, potentially allowing surgeons to identify the specific type of brain tumor they encounter, and to delineate its margin during real-time surgical procedures, enabling full removal while sparing normal brain tissue.
Summary
Gliomas are tumors occurring in the brain or spinal cord. They are difficult to treat as they lack clear edges, which complicates full surgical removal. This leads to high levels of recurrence and mortality. However, previous findings have identified a particular mutation very common in gliomas but rare in other cancers and in normal tissue.
Dr. Atsushi Natsume, Department of neurosurgery, Nagoya University Graduate School of Medicine (Dean: Masahide Takahashi, M.D., Ph.D.), and colleagues develops a device for quick, accurate identification of a mutation strongly associated with a cancer that affects the central nervous system, potentially enabling accurate removal of the entire tumor during an operation.
Research Background
Gliomas are tumors occurring in the brain or spinal cord. They are difficult to treat as they lack clear edges, which complicates full surgical removal. This leads to high levels of recurrence and mortality. However, previous findings have identified a particular mutation very common in gliomas but rare in other cancers and in normal tissue.
Tumors must be identified with high precision, and if they are malignant, the anticipated speed they will spread is also critical to ascertain. If full excision of the tumor is planned, it is also necessary to determine where tumorous tissue ends and normal tissue begins. This is particularly important for brain tumors, as the removal of any tissue can impair key brain functions. Gliomas are difficult to treat because they expand into surrounding tissue inconsistently, blurring their margins. However, most do have a specific genetic mutation rarely found in other central nervous system cancers.
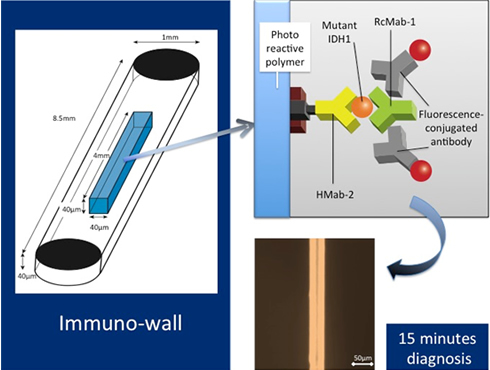 Research Results
Research Results
The researchers reported their breakthrough device, which they call an "immuno-wall microdevice," in Science and Technology of Advanced Materials. The device features a chip with an attached highly-specific antibody, HMab-2, produced by Yukinari Kato at Tohoku University that binds to the protein produced by the gene in which the mutation has occurred. When a sample containing the mutated protein is added to the device, the protein binds to the antibody, which is then specifically detected by a source of fluorescence. In contrast, if the sample is from normal tissue without this mutation, or is from a tumor other than a glioma, no fluorescence occurs.
The immuno-wall determines whether a sample is positive for a specific mutation in the isocitrate dehydrogenase 1 gene, which is present in around 70%-80% of grade II and III gliomas. The results for a range of cancerous cell lines and actual tumor samples both positive and negative for this mutation were very promising. The device was proven highly accurate, as confirmed by complete sequencing of the gene in question in each sample.
The small sample size required for the device reduces the invasiveness of sample harvesting. In fact the process takes only 15 minutes, enabling completion during an operation. The immuno-wall could markedly increase success of glioma treatment by rapidly providing data to inform the course of the operation and tissue to remove.
Research Summary and Future Perspective
The data indicate that a sample with just 500 cells or 500 ng of protein is sufficient to give a positive result. The key to success in the immuno-wall assay is that we luckily have HMab-2, the highly-specific antibody to the mutant IDH1. This means the immuno-wall can identify the margins of tumors where only low numbers of cancerous cells are present. Alternatively, sampling could even involve only obtaining blood or cerebrospinal fluid, rather than removing brain tissue, making the procedure even less invasive.
Article
Akane Yamamichi, Toshihiro Kasama, Fumiharu Ohka, Hiromichi Suzuki, Akira Kato, Kazuya Motomura, Masaki Hirano, Melissa Ranjit, Lushun Chalise, Michihiro Kurimoto, Goro Kondo, Kosuke Aoki, Noritada Kaji, Manabu Tokeshi, Toshio Matsubara, Takeshi Senga, Mika K. Kaneko, Hidenori Suzuki, Toshihiko Wakabayashi, Yoshinobu Baba, Yukinari Kato, Atsuhi Natsume. An immuno-wall microdevice exhibits rapid and sensitive detection of IDH1-R132H mutation specific to grade II and III gliomas. Science and Technology of Advanced Materials, Oct.4, 2016.
DOI: 10.1080/14686996.2016.1227222
The article was supported by a Grant-in Aid for Scientific Research on Innovative Areas from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by the priority research project of "The knowledge hub of AICHI" and by Practical Research for Innovation Cancer Control from Japan Agency for Medical Research and development, AMED; the Platform for Drug Discovery, Informatics, and Structural Life Science from AMED.
4. Establishment of a novel preoperative brain mapping system by navigated transcranial magnetic stimulation (nTMS).
Project leader: Kazuya MOTOMURA MD, PhD
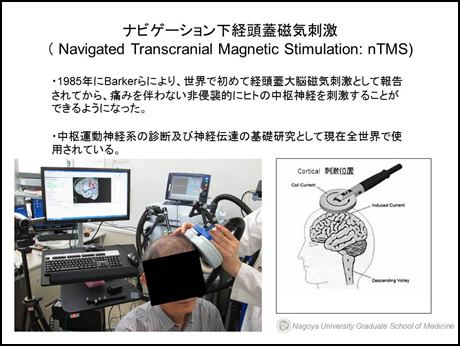 We perform awake brain mapping for safe and maximum resection of tumors with the simultaneous preservation of brain functions, in the eloquent areas of language, motor and higher function, and in their vicinity. The biggest advantage of awake brain mapping is direct functional evaluation of a certain area, making it possible to prevent post-operative language and higher brain function disorders. Although faster and safe awake surgical mapping would be possible if information on brain function before surgery could be obtained, a non-invasive high precision pre-operative brain function test as such is not available at present.
We perform awake brain mapping for safe and maximum resection of tumors with the simultaneous preservation of brain functions, in the eloquent areas of language, motor and higher function, and in their vicinity. The biggest advantage of awake brain mapping is direct functional evaluation of a certain area, making it possible to prevent post-operative language and higher brain function disorders. Although faster and safe awake surgical mapping would be possible if information on brain function before surgery could be obtained, a non-invasive high precision pre-operative brain function test as such is not available at present.
There is no evidence that pre-operative brain mapping with functional MRI correctly predicts that a certain area of the brain is actually used to perform those certain tasks.
That area of the brain might only be slightly associated with a certain task, thus making pre-operative assessment incomplete.
Transcranial magnetic stimulation (TMS) is a magnetic method used to stimulate nerves and small regions of the brain. So far, rTMS has already been approved for treatment of refractory depression in Canada, Israel and the USA. In Japan, reports of outcomes with TMS have increased, especially in the recent years after the first safety guidelines were published in 1998. In this study, we use a non-invasive next generation instrument called navigation TMS (nTMS) to accurately identify language, motor and higher brain function areas pre-operatively. Moreover, with comparative analysis with the fMRI and the results of awake surgery, we plan to develop an accurate method to identify language, motor, higher brain functions and dominant hemisphere pre-operatively.
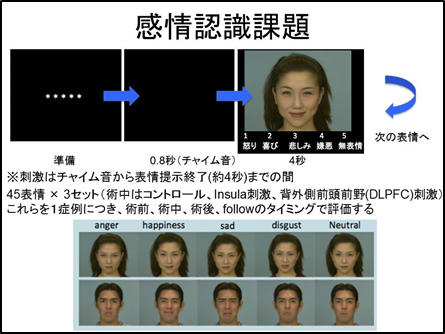
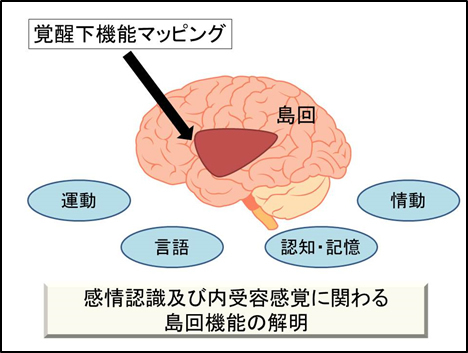
5. Investigate the insular function associated with the emotional and interoceptive awareness and using a brain mapping study. Project leader: Kazuya MOTOMURA MD, PhD
There has been a lot of research on how the brain and the body functions to recognise one's feelings. It has been considered from the research so far that the insular cortex is responsible for somatesthesia, especially in processing visceral sensation. Also, our research collaborators Terasawa, Umeda and others have analyzed brain functions in brain injury cases with neurophysiological methods and functional MRI to understand social and emotional cognitive mechanisms. They reported that the activities of the insular cortex increases in cases of interoceptive senses and in emotionally awake state of subjective senses. Therefore, to experience emotions, interoceptive senses play an important role and insular cortex may function as its nerve center. In this study, by directly stimulating insular cortex and white matter while employing recognition of facial expression tasks and monitoring heart rate during awake surgery for tumors of insular cortex and neighboring areas, we aim to define the roles and functions of the insular cortex in emotional cognition and interoceptive sensation.
6. CSF protein and genetic analysis of Moyamoya Disease; Project leader: Yoshio ARAKI, MD, PhD
We have previously published 2 original research papers on cerebrospinal fluid proteins of Moyamoya disease (MMD) patients. We analyzed and compared the CSF protein (peptides) in MMD and other diseases and discovered 2 types of peptides (m/z4473と m/z4588)that were significantly increased in MMD. (Araki et al. BMC Neurology 2010, 10:112).
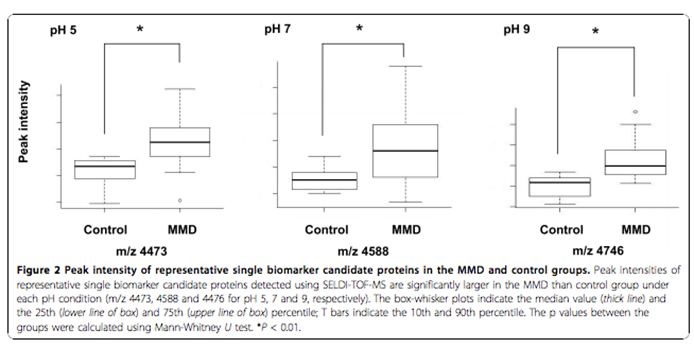
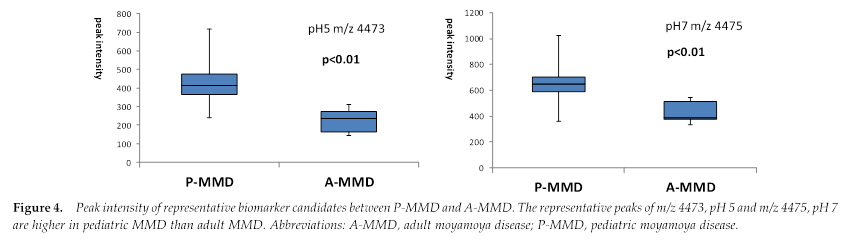
In a follow up research, we reported that m/z4473 was particularly high in pediatric moyamoya patients and gradually decreases with age. (Maruwaka et al. Journal of Stroke and Cerebrovascular Diseases, Vol. 24, 2015: pp 104-111)
We are currently investigating the functions of these peptides. We are also conducting genetic analysis of CSF of moyamoya patients and control groups to discover genes responsible for MMD pathology.
7. Elucidation of nNOS phosphorylation regulating mechanism in the hippocampal neural cells during Subarachnoid hemorrhage. Project leader: Yoshio ARAKI, MD, PhD
Nitric oxide (NO), produced from L-arginine by NOS (nitric oxide synthase), not only functions as a neurotransmitter but is also produced in the endothelium and is known to increase local blood flow through vasodilation.
Our research collaborator Prof. Osuka Koji (Aichi Medical University) has been investigating the relationship between CaMK II activation and phosphorylated neuronal NOS (p-nNOS) in ischaemic and SAH rat models. P-nNOS is up/down regulated by NO synthesis. We want to explain the following by investigating changes in hippocampal p-nNOS caused by post SAH acute increase in intracranial pressure.
a) Whether p-nNOS at Ser is present in the hippocampus in the early phase of SAH rat model.
b) Whether it is dependent on AMP-dependant protein kinase activation.
c) How does CaMK II activated p-nNOS at Ser847 and PKA activated p-nNOS at Ser1412 influence early brain injury in the hippocampus in the early phase of SAH?
This research aims to explain the neuroprotective mechanism of NOS phosphorylation in the hippocampus immediately after SAH. Hopefully it can be used to prevent post SAH higher cognitive function disorder by inhibiting early brain injury after SAH.
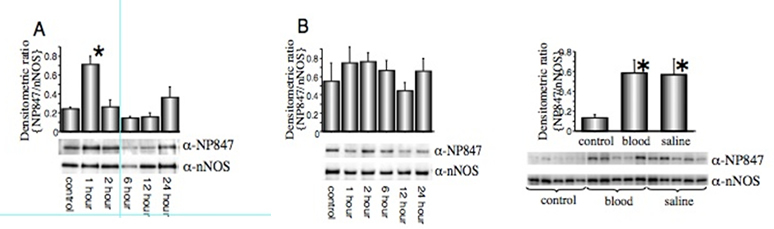
p-nNOS at Ser847 is increased due to CaMK II activation in hippocampal cells 1 hour after induction of Rat SAH model. (Makino et al. Brain Res. 2015)
8. Higher Brain function network analysis and development of next-generation epilepsy surgery by using fMRI、EEG-fMRI、and MEG. Project leader: Satoshi MAESAWA, MD, PhD
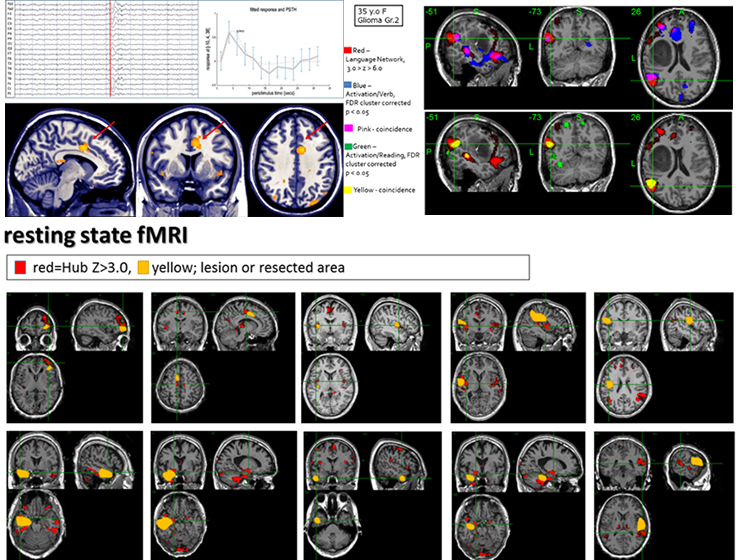
We aim to develop safer and more effective surgical procedures by utilizing the neural network information generated by latest modalities like resting state fMRI, DTI tractography and MEG. We introduced a novel EEG-f MRI simultaneous recording device, diagnosed the focus of epilepsy and performed network analysis. EEG-fMRI analysis shows inter-ictal BOLD activities near epileptic focus (pic: up left). Resting fMRI network analysis shows increase in epileptic abnormal connections (pic: up right). From the findings of awake surgical mapping, we studied functional preservation from hodological point of view and observed basic network change and sub-cortical linguistic network of default mode network from resting network analysis. We compared resting fMRI of linguistic network and fMRI with task (pic: up right) and by comparative study of results of electric stimulation mapping during surgery, we are pursuing non-invasive and more accurate pre-operative evaluation of brain function by understanding neural foundation. We operate in coordination with Nagoya University Brain and Mind Research Centre.
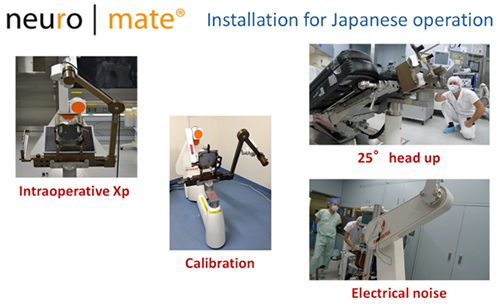
9. Clinical application of stereotactic brain surgery with Neuromate® robot. Project leader: Daisuke NAKATSUBO
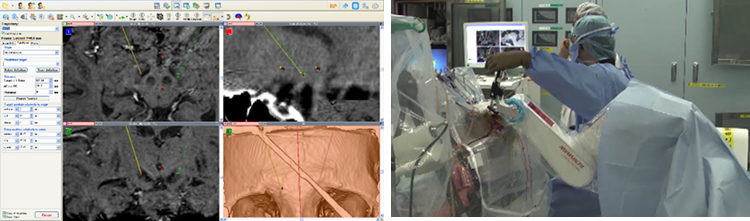
NeuroMate is a computer-controlled, robotic system for stereotactic functional brain surgeries. A highly precise and safe targeting by the application of robotics promises improvement in accuracy and effectiveness of stereotactic surgery. Neuromate, a CE mark and FDA approved technology, received pharmaceutical approval in Japan in June 2015. It has been modified to fit Japanese surgical techniques and we have applied it to deep brain stimulation (DBS) for parkinsons disease in a clinical trial of 8 cases. We have confirmed its efficacy and verified its precision with existing stereotactic frame system (fig above). After its pharmaceutical approval, it has mostly been used in DBS. At Nagoya University, in coordination with the department of Radiology, we perform planning based on direct imaging with 3T MRI (Fig left below). With Neuromate, it is possible to make detailed verification of neural activities of basal ganglia by microelectrode recording (MER) during surgery (fig right below). We also use Neuromate to place multiple electrodes for focal diagnosis. We plan to broaden its application by frameless system installation and workstation improvisation. By collaborating with image analysis technology like EEG-fMRI of BMRC, we are proceeding with the verification of our research results.
10. Treatment of tremor by MRI guided focused ultrasound
Project leader: Satoshi MAESAWA, MD, PhD, Daisuke NAKATSUBO, Shoko KATO
Project leaders: Maesawa Satoshi, Nakatsubo Daisuke, Kato Shoko
Focused ultrasound (FUS) is a therapeutic instrument that focuses ultrasound energy on a single place and treats the lesion by increasing its temperature. Non-invasive temperature mapping is possible with MRI and can be used effectively with FUS that uses heat coagulation as its main mechanism of action thus making it possible to assess treatment efficacy and side effects during surgery. The MRgFUS is a revolutionary treatment that combines focused ultrasound and MRI. A helmet with 1024 probes is equipped in a bed specially designed for FUS. The patient wears the helmet and enters the MRI machine. The ultrasound waves generated from the ultrasound probe are focused to the precise region of the brain and cause the temperature of that region to increase thus bringing the therapeutic effect. Insightec's neurosurgery solution, Exablate Neuro, is the first focused ultrasound device approved by the FDA in July 2016. Exablate Neuro is in the process of PMDA for approval in Japan to treat patients with essential tremors and parkinsons disease. 15 patients in Virginia university underwent Vim ablation for essential tremors, and its efficacy and safety has been verified in the clinical study results. It has also been found to be effective in tremors in parkinsons disease by targeting PTT. Besides these, its application is expected in trigeminal neuralgia, malignant brain tumors, and cerebrovascular diseases. At present (August 2016), 5 such systems have been installed so far and it is soon going to be installed in a Nagoya University Department of Neurosurgery affiliated hospital too. We plan to proceed with the efficacy study of this non-invasive technology of MRgFUS for essential tremor and Parkinson disease.
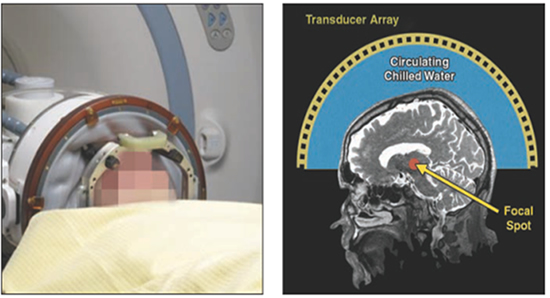
(Elias WJ,2011 NEJM)
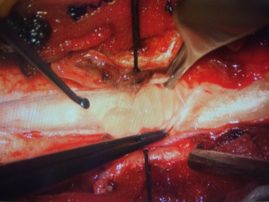
11. Spine Group Research Project: Project leader Nishimura Yusuke
1. Less invasive spine surgery;
We have been practicing and studying the clinical outcomes of less invasive surgery to minimize the injury to normal structures of skin and muscles.
- Anterior cervical decompression
We treat cervical radiculopathy with a 6 mm small hole drilled with the assistance of surgical microscope and without placing any artificial implants. With this technique, inter-vertebral mobility is preserved and risk of degenerative change to the adjacent vertebra is minimized. We have reported good clinical outcomes and vertebral stability using finite element method. At present we are studying post-operative change in the alignment of the vertebrae, stability of the operated vertebra through radio-imaging, and influence on the adjacent vertebra.
- Posterior lumbar fixation with Wiltse approach
In Wiltse approach, the lateral side of the facet is approached by dissecting between muscles causing minimal muscular damage. With this approach screw placement is possible with almost no muscular damage, and we have been studying the clinical outcome of its application in thoraco-lumbar posterior fixation. Compared to conventional methods, similar treatment effects have been achieved with less blood loss and less post-operative pain. We are studying the results of further minimization of surgical invasion by combining it with oblique lumbar interbody fusion (OLIF).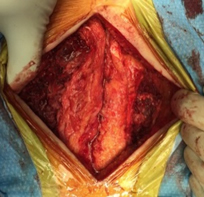

2. Intraoperative nerve monitoring (MEP ; motor evoked potentials , SEP ; somatosensory evoked potentials) ; Project leader Nishimura Yusuke
We use intraoperative nerve monitoring in all of our spinal cases and check MEP and SEP to make the surgery as safe as possible. Sometimes the intraoperative wave changes can be false positives. We have used animal models (rats and mice) to analyze and predict reasons behind the false positives and have already reported blood pressure as a significant factor. We are now studying the effects of blood pressure to MEP waves in detail.
3. Treatment of Vertebral and Spinal Tumor.
- Surgical outcomes of spinal intramedullary tumors
We apply minimally invasive techniques to prevent post operative spine deformity, to minimize the risk of post operative palsy and sensory disorder. We also conduct genetic analysis of the pathological specimens with special consideration to the difference in the genetics of spinal and brain tumors. -
 Surgical outcomes of spinal extramedullary tumors
Surgical outcomes of spinal extramedullary tumors
Surgical indication for tumor resection and spinal fixation for malignant spinal tumors including metastatic spinal tumors have broadened with our less invasive surgical techniques. Surgical outcomes are improving and we are studying them in detail. We coordinate with the tumor group of the orthopedic department of Aichi Cancer Centre and have removed complicated tumors with combined effort of different faculties.
4. Basic research of spinal nerve regeneration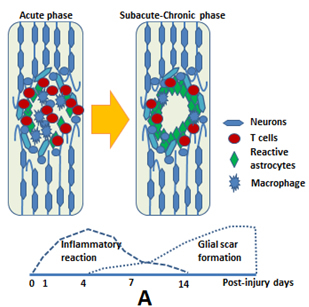 We have reported the immensely significant role of microglia in central nerve immune-response (Takeuchi et al. Experimental Neurology 2008). In a more recent study we reported that the motor function recovery by IFN-β transduced neural stem cells in spinal injury mouse is delivered through glial scar inhibition; but microglial aggregation to the injury site is decreased at the same time (Fig C) (Nishimura et al. Cell transplantation 2012, Ito et al. J of Neurotrauma 2009). Motor function improvement can be obtained with microglial inhibition (Umebayashi et al. J Neurotrauma. 2014). Now, we are focusing on autoimmune response after spinal cord injury and working towards spinal regeneration with this autoimmune inhibition.
We have reported the immensely significant role of microglia in central nerve immune-response (Takeuchi et al. Experimental Neurology 2008). In a more recent study we reported that the motor function recovery by IFN-β transduced neural stem cells in spinal injury mouse is delivered through glial scar inhibition; but microglial aggregation to the injury site is decreased at the same time (Fig C) (Nishimura et al. Cell transplantation 2012, Ito et al. J of Neurotrauma 2009). Motor function improvement can be obtained with microglial inhibition (Umebayashi et al. J Neurotrauma. 2014). Now, we are focusing on autoimmune response after spinal cord injury and working towards spinal regeneration with this autoimmune inhibition.
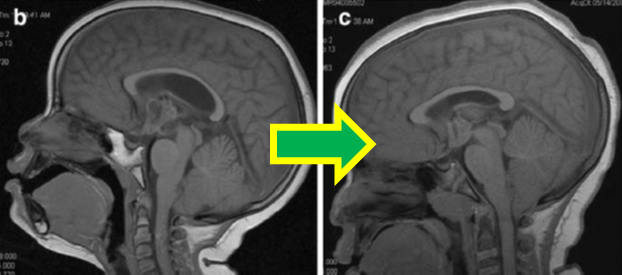
12. Secondary premature craniosynostosis after brain tumor treatment:Iatrogenic risk factors and diagnostic markers of Chiari malformation.
Project leader Goro KONDO, Michihiro KURIMOTO (Collaborators: Mihiko KATO, Hirokatsu OHSAWA
Secondary craniosynostosis is premature synostosis occurring during the course of some other disease and treatment, with most of it arising in cases of excessive shunting, causing growth arrest of cranium and subsequent deformity and decrease in intracranial volume. Special consideration is required in brain tumor cases because of higher chances of shunt placement for hydrocephalus in these cases. Moreover, craniosynostosis after radiation therapy may cause complicated cranial deformation, and chiari malformation like changes have been reported in posterior fossa irradiation. Surgical management is not always easy, so preventive strategy is very important. We are studying the relevant risk factors and diagnostic markers with special focus on serum ALP level because of its role in bone formation. Among pediatric patients admitted to our department since 2013, we studied 40 brain tumor resection patients and found that 26 of them presented with hydrocephalus and 11 (26.3%) developed secondary craniosynostosis. In contrast, 14 patients with no hydrocephalus didn not develop craniosynostosis. Among craniosynostosis cases, 5 patients (45.5%) underwent shunt placement surgery. All the craniosynostosis cases had high ALP level for a certain period of time and the course was compatible with synostosis progress during that time period. As a result it was shown that preoperative hydrocephalus is a risk factor for post tumor resection secondary craniosynostosis(P<0.01). We believe this proves that not only continuous CSF drainage (shunt) but also decrease in intracranial pressure with a single surgery may cause secondary craniosynostosis.
Although there are also several reports on developmental retardation after radiation therapy in pediatric patients, knowledge of secondary microcephaly and cranisynostosis is scarce. However, with 40% patients developing secondary craniostynostosis, influence on development of brain tumor survivors is worth studying. Therefore, change in the shape of the cranium should also be noted during follow up after brain tumor removal surgery, especially in cases with initial presentation of hydrocephalus. Minimal radiological changes may be difficult to observe; but blood ALP levels could be useful diagnostic markers. We plan to continue our study by with more number of cases.
(fig b:before treatment、c:after treatment(worsening tendency)
13. Efficacy of temozolomide/irinotecan/bevacizumab triple combination therapy for recurrent medulloblastoma and search for predictive biomarkers. Project leader Goro KONDO, (Collaborators: Brain tumor group Atsushi NATSUME, Kazuya MOTOMURA, Fumiharu OHKA)
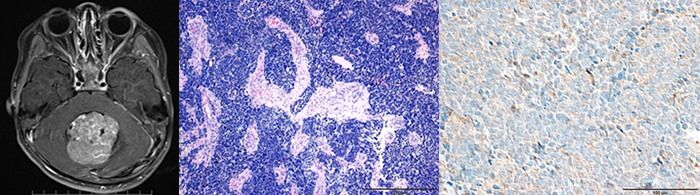
Standard treatment for recurrent medulloblastoma hasn`t been established yet. Until now, treatment of recurrent medulloblastoma included Temozolomide (Cefalo et. al.Neuro Oncol 16:748-53, 2014),TMZ plus CPT11V (Grill et. al.) which had lower response rate than Cefalo et al possibly because of lower TMZ doses, reversely proving the case for significance of TMZ(Neuro Oncol 15:1236-1243, 2013). Aguilera et. al. combined CPT11 and bevacizumab(Bev) and reported long term survival proving efficacy of CPT11/BEV(Pediatr Blood Cancer 56:491-494, 2011). After that TMZ/CPT11/Bev triple drug therapy was reported and it showed the highest response rate(55.6%) compared to the previous regimens(Childs Nerv Syst 29:589-596, 2013). Thus, Temozolomide(TMZ)/ irinotecan (CPT11)/ bevacizumab(Bev) triple therapy may become the standard treatment of the future. At present we are studying the efficacy of this protocol as the possible standard treatment for recurrent medulloblastoma in our hospital.。So far, we have studied the pathological findings and biomarkers of 4 patients who were administered this regimen and searched for prognostic factors. Pathologically it can be divided into 4 subclasses namely, desmoplastic/nodular、MBEN、classic、anaplastic / large cell (LCA). Although sub-classification based on genetic analysis is widely used recently、there is no understanding on prognostic factor of TMZ/CPT11/BEV treatment. We use immune-histological findings of cases treated in our hospital to comprehensively search for possible biomarkers including VEGF.(Attached fig: 1)Medulloblastoma image(MRI T1WI Axial view Gd(+))、2)medulloblastoma patho-histological picture(HE stain)、2)Medulloblastoma immunohistostaining VEGF(+))case)
14. Endoscopic/ Pituitary Group Research Projects: Project leader: Kazuhito TAKEUCHI
1. Development of novel endoscopic surgical techniques and peripheral equipment for intracranial lesions.
Surgical treatment using an endoscope is becoming more and more common in the neurosurgical field these days. Trans-nasal endoscopic pituitary tumor resection was first reported about 20 years ago and is an area that will further develop in the future. To use this surgical technique in larger tumors less invasively, it is necessary to develop new surgical approaches and equipment. The goal of this project is as follows.
a. Widening the indications of endoscopic trans-nasal trans-sphenoidal, approach and equipment development
Trans-nasal trans-sphenoidal approach is already being used in different hospitals for pituitary tumors, tuberculum sella meningioma, craniopharyngioma, chordoma etc. With this surgical method, approach to the lesions is possible without touching the normal brain, thus is a very less invasive procedure. However, because manipulating space is limited in the surgery through the nasal cavity, surgical manipulation becomes more difficult as you move lateral from the central axis. By deepening our knowledge of the nasal cavity and developing novel nasal cavity techniques, we are developing techniques and tools to make this surgical method even further less invasive and widen its indication for larger tumors. Special equipment are necessary for this surgery, for example, it is necessary to develop forceps that can bend and rotate in deep seated locations. We have started surgical equipment development in cooperation with other universities and enterprises and have been successful in its partial productization.
b. Application of endoscopic surgery for brain tumors and equipment development
We are developing surgeries to remove brain lesions by applying endoscopic skull base techniques. A 6-12mm small clear tube is inserted toward the lesion, thereby minimizing damage to the peritumoral normal brain parenchyma by to doing the complete tumor excision within the cylinder itself. Although it is possible to make brain tumor surgery less invasive, it is necessary to develop special device for the new surgical methods. We plan to develop these surgical techniques and tools and make them available for worldwide use in the future.
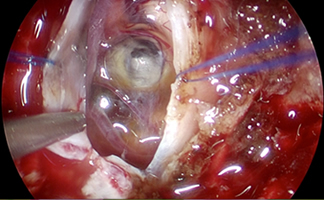
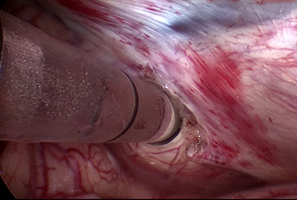
Application of nasal surgery to brain stem lesion. Brain tumor surgery using clear sheath.
Basic research
- Study on hydrocephalus pathogenesis using ciliary dyskinesia mouse models.
Congenital hydrocephalus is a group of diseases that is often encountered in pediatric neurological practice. Among congenital hydrocephalus, one with no obvious occlusion is called communicating hydrocephalus, one of the reasons for which is failure of ciliary movement present in the ependymal cells. Cilia is present in cell surface of various tissues like bronchus, fallopian tube, ventricles, etc. Cilia presents with a characteristic9+1structure and is involved in the transport of substances on the surface made possible with a periodic rotary motion by the sliding movement of dynein. It is possible to know the origins of hydrocephalus by using the pili movement disorder model mouse. Along with the site of impaired spinal fluid reflux by impairment of ciliary motion, we are also studying ciliary motility in normal mice to learn how cilia contributes to the formation of cerebrospinal fluid circulation.
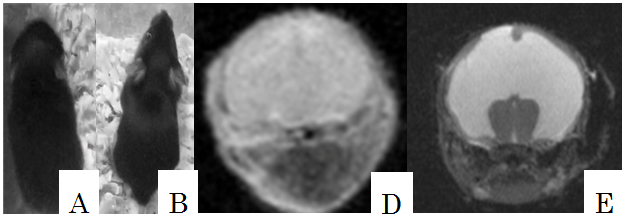
A、B: Hydrocephalus and normal mouse. Head circumference is expanded.
D、E:MRI image of hydrocephalus and normal mouse. Expanded ventricles can be observed.
15. Endovascular Neurosurgery Research Projects: Project leader: Takakashi IZUMI
Basic research
To resolve the questions that arise from our daily clinical practice, we have been developing experimental systems that serve as a model to prove our clinical practice. The experimental models not only give us hints on solving our clinical questions but also serve to improve endovascular neurosurgery by helping us develop new treatment methods which we again apply in our clinical practice. We are currently conducting the following clinically applicable basic research.
- Safety of intracranial stent occlusion in silicon and animal model.
We confirmed the feasibility and safety of intracranial stent occlusion in a silicon model. To verify its safety in vivo, we placed the stent in a rabbit model and verified the safety of the stent occlusion when it was covered with neo-intima. - Catheter traction comparative experiments in silicon model
Micro-catheter, when injected with liquid embolic substance such as NBCA or ONYX, may result in adhesion and may be difficult to remove and break off on pulling. Additional surgical invasion for its removal might be required. Only a small portion of the tractive force applied while pulling out the micro-catheter is transmitted to its distal end because of meandering of the blood vessel. There are also differences depending on the material of the micro-catheter. We are comparing and verifying these differences in silicon models.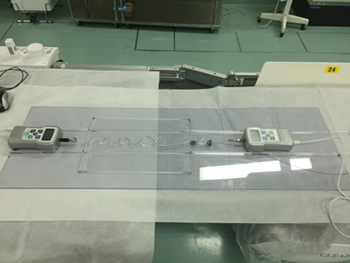
- Observation of the coil behavior in aneurysm coil embolization
There are various features in the coils used for embolization of aneurysm.
To understand the characteristics of the respective coils, we are doing observational experiment using various coil movement models, which would be difficult to observe during a normal endovascular surgery. We are studying the behavior and filling rate of filling and finishing coils in model case scenarios with varying aneurysm shape and size.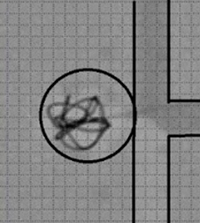
- Study of pressure on the vessel at the time of balloon expansion during endovascular treatment. In endovascular surgery, balloon assist may be used to prevent coil prolapse. However, balloon expansion may also cause vascular damage. We use silicon vascular models to measure expanded balloon pressure and to choose safe balloons and develop safer expansion techniques.
Fig: A portion of the balloon bulges after it is expanded inside a silicon tube.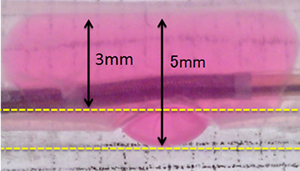
Clinical Research
- Correlation between spinal dural arteriovenous fistula and degenerative diseases.
The comorbidity of the spinal cord dural arteriovenous fistula and spinal degenerative disease was analyzed, including the correlation with the vein occlusion. Concomitant ipsilateral hernia or osteophytes were found in high rates. Furthermore, high rates of concomitant vein occlusion was also observed. We believe that these findings suggest a correlation with the genesis of spinal dural arteriovenous fistula. - Study of recurrence factor of unruptured brain aneurysm.
We are analyzing the factors like size and location of aneurysms in our vast number of cases of unruptured aneurysm treatment. While the size coil density of the aneurysm was significantly correlated with recurrence, we did not find any advantages with thick primary coil diameter. - Study of risk factors for stenting in cervical carotid artery stenosis
Treatment of carotid artery stenosis includes carotid endarterectomy (CEA: direct surgery) and stenting (CAS: an endovascular treatment). On the basis of the accumulated data in our hospital, we are studying the high-risk factors of the cases treated with CAS to develop safer treatment policies. - Study of the optimal antiplatelet therapy as observed from long-term results of stent assisted coil embolization of brain aneurysms.
Stent assisted coil embolization for brain aneurysms is becoming the main stream treatment. However, dual antiplatelet therapy is a must in these stent cases. During long term follow up, the optimal timing to reduce antiplatelet to a single tablet (DAPT-ACE study in progress) and whether antiplatelet can be stopped altogether is still a matter of debate. We are studying our cases to find out the right answer and also analyzing ischemic and hemorrhagic complications and their risk factors. - Study of puncture site bleeding after the cerebral endovascular treatment
Puncture site bleeding prolongs bed rest time after endovascular surgery and is a major risk factor for longer hospital stay. Pseudo-aneurysm may occur and surgical intervention might also be required in some cases. We did a retrospective study on the risk factors and on how to shorten bed rest and hospital stay, and as a result, endovascular treatment became safer and hospital stay shortened. - Study of the position of the shunt pouch in dural arteriovenous fistula of the cavernous sinus.
There is a need to accurately identify the shunt pouch in order to do a super-selective embolization of the dural arteriovenous fistula. We are retrospectively analyzing the distribution of the opening of shunt pouch of the sinus.
Faculty Members
| Faculty | Position | Department |
|---|---|---|
| Ryuta SAITO | Professor | |
| Atsushi NATSUME | Associate professor | Brain Tumor Surgery |
| Takashi IZUMI | Associate professor | Neuroendovascular surgery |
| Kazuya MOTOMURA | Associate professor | Brain Tumor Surgery |
| Satoshi MAESAWA | Associate professor | Brain and Mind Research Center |
| Sho OKAMOTO | Associate professor | Neurovascular Surgery |
| Yusuke NISHIMURA | Associate professor | Spinal surgery |
| Daisuke NAKATSUBO | Associate professor | Functional neurosurgery |
| Yoshio ARAKI | Assistant professor | Neurovascular Surgery |
| Fumiharu OHKA | Assistant professor | Brain Tumor Surgery |
| Kazuhito TAKEUCHI | Assistant professor | Neuroendoscopy |
| Kuniaki TANAHASHI | Assistant professor | Brain Tumor Surgery |
| Kosuke AOKI | Assistant professor | Brain Tumor Surgery |
| Goro KONDO | Assistant professor | Pediatric Neurosurgery |
| Kaoru EGUCHI | Assistant professor | Spinal surgery |
| Michihiro KURIMOTO | Assistant professor | Pediatric Neurosurgery |
| Masahiro NISHIHORI | Assistant professor | Neuroendovascular surgery |
Bibliography
- 2016
- Takeuchi K, Watanabe T, Nagatani T, Nagata Y, Chu J, Wakabayashi T. Incidence and risk factors of subdural hematoma after intraoperative cerebrospinal fluid leakage during the transsphenoidal approach. Pituitary, 2016.
- Nagata Y, Takeuchi K, Kato M, Osawa H, Watanabe T, Wakabayashi T. The "steppingstone" phenomenon: a new endoscopic finding in slit-ventricle syndrome. Childs Nerv Syst, 2016.
- Nagata Y, Takeuchi K, Kato M, Chu J, Wakabayashi T. Lateral temporal encephaloceles: case-based review. Childs Nerv Syst, 2016; 32: 1025-1031.
- Muraoka S, Araki Y, Izumi T, Takeuchi K, Okamoto S, Wakabayashi T. Cerebral Infarction and Subarachnoid Hemorrhage Caused by Central Nervous System Aspergillus Infection. World Neurosurg, 2016; 90: 705.e709-705.e713.
- Maesawa S, Bagarinao E, Fujii M, Futamura M, Wakabayashi T. Use of Network Analysis to Establish Neurosurgical Parameters in Gliomas and Epilepsy. Neurol Med Chir (Tokyo), 2016; 56: 158-169.
- Shiina S, Ohno M, Ohka F, Kuramitsu S, Yamamichi A, Kato A, Motomura K, Tanahashi K, Yamamoto T, Watanabe R, Ito I, Senga T, Hamaguchi M, Wakabayashi T, Kaneko MK, Kato Y, Chandramohan V, Bigner DD, Natsume A. CAR T Cells Targeting Podoplanin Reduce Orthotopic Glioblastomas in Mouse Brains. Cancer Immunol Res, 2016; 4: 259-268.
- Kurimoto M, Suzuki H, Aoki K, Ohka F, Kondo G, Motomura K, Iijima K, Yamamichi A, Ranjit M, Wakabayashi T, Kimura S, Natsume A. Rapid sensitive analysis of IDH1 mutation in lower-grade gliomas by automated genetic typing involving a quenching probe. Cancer Invest, 2016; 34: 12-15.
- Nagata Y, Takeuchi K, Nagatani T, Watanabe T, Sato Y, Tambara M, Wakabayashi T. Bilateral occlusion of the foramina of Monro after endoscopic third ventriculostomy for aqueductal stenosis--a case report. Childs Nerv Syst, 2016; 32: 739-743.
- Maesawa S, Fujii M, Futamura M, Hayashi Y, Iijima K, Wakabayashi T. A case of secondary somatosensory epilepsy with a left deep parietal opercular lesion: successful tumor resection using a transsubcentral gyral approach during awake surgery. J Neurosurg, 2016; 124: 791-798.
- Asai T, Miyachi S, Izumi T, Matsubara N, Haraguchi K, Yamanouchi T, Ota K, Shintai K, Tajima H, Wakabayashi T. Relationship between low response to clopidogrel and periprocedural ischemic events with coil embolization for intracranial aneurysms. J Neurointerv Surg, 2016; 8: 752-755.
- Motomura K, Chalise L. [Update Knowledge for Brain Tumors(9)Peripheral Nerve Tumor]. No Shinkei Geka, 2016; 44: 699-709.
- Motomura K NA, Iijima K, Kuramitsu S, Fujii M, Yamamoto T, Maesawa S, Sugiura J, Wakabayashi T. Surgical benefits of combined awake craniotomy and intraoperative magnetic resonance imaging for gliomas associated with eloquent areas. J Neurosurg, 2016; in press.
- 2015
- Kajita Y, Nakatsubo D, Kataoka H, Nagai T, Nakura T, Wakabayashi T. Installation of a Neuromate Robot for Stereotactic Surgery: Efforts to Conform to Japanese Specifications and an Approach for Clinical Use-Technical Notes. Neurol Med Chir (Tokyo), 2015; 55: 907-914.
- Takeuchi K, Nagatani T, Wakabayashi T. How I do it: shoelace watertight dural closure in extended transsphenoidal surgery. Acta Neurochir (Wien), 2015; 157: 2089-2092.
- Yamamuro S, Sano E, Okamoto Y, Ochiai Y, Ohta T, Ogino A, Natsume A, Wakabayashi T, Ueda T, Hara H, Nakayama T, Yoshino A, Katayama Y. Antitumorigenic effect of interferon-beta by inhibition of undifferentiated glioblastoma cells. Int J Oncol, 2015; 47: 1647-1654.
- Momota H, Kato S, Fujii M, Tsujiuchi T, Takahashi Y, Kojima S, Wakabayashi T. Primary peripheral T-cell lymphoma, not otherwise specified, of the central nervous system in a child. Brain Tumor Pathol, 2015; 32: 281-285.
- Tsuboi T, Watanabe H, Tanaka Y, Ohdake R, Yoneyama N, Hara K, Ito M, Hirayama M, Yamamoto M, Fujimoto Y, Kajita Y, Wakabayashi T, Sobue G. Characteristic laryngoscopic findings in Parkinson's disease patients after subthalamic nucleus deep brain stimulation and its correlation with voice disorder. J Neural Transm (Vienna), 2015; 122: 1663-1672.
- Takanari K, Araki Y, Okamoto S, Sato H, Yagi S, Toriyama K, Yokoyama K, Murotani K, Matsui S, Wakabayashi T, Kamei Y. Operative wound-related complications after cranial revascularization surgeries. J Neurosurg, 2015; 123: 1145-1150.
- Ranjit M, Motomura K, Ohka F, Wakabayashi T, Natsume A. Applicable advances in the molecular pathology of glioblastoma. Brain Tumor Pathol, 2015; 32: 153-162.
- Tanahashi K, Natsume A, Ohka F, Motomura K, Alim A, Tanaka I, Senga T, Harada I, Fukuyama R, Sumiyoshi N, Sekido Y, Wakabayashi T. Activation of Yes-Associated Protein in Low-Grade Meningiomas Is Regulated by Merlin, Cell Density, and Extracellular Matrix Stiffness. J Neuropathol Exp Neurol, 2015; 74: 704-709.
- Tanei T, Kajita Y, Wakabayashi T. [Pharmacological treatment and neuromodulation therapy for central neuropathic pain: current trend and issue of spinal cord stimulation]. No Shinkei Geka, 2015; 43: 507-515.
- Makino K, Osuka K, Watanabe Y, Usuda N, Hara M, Aoyama M, Takayasu M, Wakabayashi T. Increased ICP promotes CaMKII-mediated phosphorylation of neuronal NOS at Ser(8)(4)(7) in the hippocampus immediately after subarachnoid hemorrhage. Brain Res, 2015; 1616: 19-25.
- Ohkawa Y, Momota H, Kato A, Hashimoto N, Tsuda Y, Kotani N, Honke K, Suzumura A, Furukawa K, Ohmi Y, Natsume A, Wakabayashi T, Furukawa K. Ganglioside GD3 Enhances Invasiveness of Gliomas by Forming a Complex with Platelet-derived Growth Factor Receptor alpha and Yes Kinase. J Biol Chem, 2015; 290: 16043-16058.
- Suzuki H, Aoki K, Chiba K, Sato Y, Shiozawa Y, Shiraishi Y, Shimamura T, Niida A, Motomura K, Ohka F, Yamamoto T, Tanahashi K, Ranjit M, Wakabayashi T, Yoshizato T, Kataoka K, Yoshida K, Nagata Y, Sato-Otsubo A, Tanaka H, Sanada M, Kondo Y, Nakamura H, Mizoguchi M, Abe T, Muragaki Y, Watanabe R, Ito I, Miyano S, Natsume A, Ogawa S. Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet, 2015; 47: 458-468.
- Fujii M, Maesawa S, Motomura K, Futamura M, Hayashi Y, Koba I, Wakabayashi T. Intraoperative subcortical mapping of a language-associated deep frontal tract connecting the superior frontal gyrus to Broca's area in the dominant hemisphere of patients with glioma. J Neurosurg, 2015; 122: 1390-1396.
- Uozumi Y, Okamoto S, Araki Y, Izumi T, Matsubara N, Yokoyama K, Sumitomo M, Miyachi S, Wakabayashi T. Treatment of Symptomatic Bilateral Cavernous Carotid Aneurysms: Long-term Results of 6 Cases. J Stroke Cerebrovasc Dis, 2015; 24: 1013-1018.
- Hiroyuki M, Ogino J, Takahashi A, Hasegawa T, Wakabayashi T. Rhabdoid glioblastoma: an aggressive variaty of astrocytic tumor. Nagoya J Med Sci, 2015; 77: 321-328.
- Tanei T, Fujii M, Takebayashi S, Nakahara N, Wakabayashi T. [Supratentorial-infraoccipital approach supported by navigation and intraoperative magnetic resonance imaging for glioma located at the medial posterior temporal lobe: two case reports]. No Shinkei Geka, 2015; 43: 241-246.
- Matsubara N, Miyachi S, Izumi T, Yamanouchi T, Asai T, Ota K, Wakabayashi T. Results and current trends of multimodality treatment for infectious intracranial aneurysms. Neurol Med Chir (Tokyo), 2015; 55: 155-162.
- Tanaka Y, Tsuboi T, Watanabe H, Kajita Y, Fujimoto Y, Ohdake R, Yoneyama N, Masuda M, Hara K, Senda J, Ito M, Atsuta N, Horiguchi S, Yamamoto M, Wakabayashi T, Sobue G. Voice features of Parkinson's disease patients with subthalamic nucleus deep brain stimulation. J Neurol, 2015; 262: 1173-1181.
- Maesawa S, Bagarinao E, Fujii M, Futamura M, Motomura K, Watanabe H, Mori D, Sobue G, Wakabayashi T. Evaluation of resting state networks in patients with gliomas: connectivity changes in the unaffected side and its relation to cognitive function. PLoS One, 2015; 10: e0118072.
- Sugiyama M, Hasegawa H, Ito S, Sugiyama K, Maeda M, Aoki K, Wakabayashi T, Hamaguchi M, Natsume A, Senga T. Paired related homeobox 1 is associated with the invasive properties of glioblastoma cells. Oncol Rep, 2015; 33: 1123-1130.
- Maruwaka M, Yoshikawa K, Okamoto S, Araki Y, Sumitomo M, Kawamura A, Yokoyama K, Wakabayashi T. Biomarker research for moyamoya disease in cerebrospinal fluid using surface-enhanced laser desorption/ionization time-of-flight mass spectrometry. J Stroke Cerebrovasc Dis, 2015; 24: 104-111.
- Tsuboi T, Watanabe H, Tanaka Y, Ohdake R, Yoneyama N, Hara K, Nakamura R, Watanabe H, Senda J, Atsuta N, Ito M, Hirayama M, Yamamoto M, Fujimoto Y, Kajita Y, Wakabayashi T, Sobue G. Distinct phenotypes of speech and voice disorders in Parkinson's disease after subthalamic nucleus deep brain stimulation. J Neurol Neurosurg Psychiatry, 2015; 86: 856-864.
- Iwami K, Momota H, Fujii M, Natsume A, Yagi S, Toriyama K, Kamei Y, Wakabayashi T. Anaplastic meningioma with rapid growth after omental flap transposition: a case report and experimental study. Brain Tumor Pathol, 2015; 32: 137-144.
- 2014
- Tanei T, Morita Y, Yashima A, Wakita H, Takebayashi S, Nakahara N, Wakabayashi T. [Severe rhabdomyolysis and intracranial hemorrhage associated with synthetic cannabinoid: a case report]. No Shinkei Geka, 2014; 42: 867-871.
- Tanahashi K, Natsume A, Ohka F, Momota H, Kato A, Motomura K, Watabe N, Muraishi S, Nakahara H, Saito Y, Takeuchi I, Wakabayashi T. Assessment of tumor cells in a mouse model of diffuse infiltrative glioma by Raman spectroscopy. Biomed Res Int, 2014; 2014: 860241.
- Tanei T, Takebayashi S, Nakahara N, Nagatani T, Wakabayashi T. [Biopsy of brain parenchymal lesions: procedure selection and ingenuity of accurate and safety biopsy]. No Shinkei Geka, 2014; 42: 837-840.
- Nishimura Y, Hara M, Nakajima Y, Haimoto S, Yamamoto Y, Wakabayashi T. Outcomes and complications following posterior long lumbar fusions exceeding three levels. Neurol Med Chir (Tokyo), 2014; 54: 707-715.
- Umebayashi D, Hara M, Nishimura Y, Wakabayashi T. A morphologically atypical case of atlantoaxial rotatory subluxation. J Korean Neurosurg Soc, 2014; 55: 284-288.
- Takeuchi K, Nagatani T, Okumura E, Wakabayashi T. A novel method for managing water and electrolyte balance after transsphenoidal surgery: preliminary study of moderate water intake restriction. Nagoya J Med Sci, 2014; 76: 73-82.
- Momota H, Fujii M, Tatematsu A, Shimoyama Y, Tsujiuchi T, Ohno M, Natsume A, Wakabayashi T. Papillary glioneuronal tumor with a high proliferative component and minigemistocytes in a child. Neuropathology, 2014; 34: 484-490.
- Ohka F, Ito M, Ranjit M, Senga T, Motomura A, Motomura K, Saito K, Kato K, Kato Y, Wakabayashi T, Soga T, Natsume A. Quantitative metabolome analysis profiles activation of glutaminolysis in glioma with IDH1 mutation. Tumour Biol, 2014; 35: 5911-5920.
- Umebayashi D, Natsume A, Takeuchi H, Hara M, Nishimura Y, Fukuyama R, Sumiyoshi N, Wakabayashi T. Blockade of gap junction hemichannel protects secondary spinal cord injury from activated microglia-mediated glutamate exitoneurotoxicity. J Neurotrauma, 2014; 31: 1967-1974.
- Tsujiuchi T, Natsume A, Motomura K, Kondo G, Ranjit M, Hachisu R, Sugimura I, Tomita S, Takehara I, Woolley M, Barua NU, Gill SS, Bienemann AS, Yamashita Y, Toyokuni S, Wakabayashi T. Preclinical evaluation of an O(6)-methylguanine-DNA methyltransferase-siRNA/liposome complex administered by convection-enhanced delivery to rat and porcine brains. Am J Transl Res, 2014; 6: 169-178.
- Yamashita Y, Ito Y, Isomura H, Takemura N, Okamoto A, Motomura K, Tsujiuchi T, Natsume A, Wakabayashi T, Toyokuni S, Tsurumi T. Lack of presence of the human cytomegalovirus in human glioblastoma. Mod Pathol, 2014; 27: 922-929.
- Okochi Y, Nihashi T, Fujii M, Kato K, Okada Y, Ando Y, Maesawa S, Takebayashi S, Wakabayashi T, Naganawa S. Clinical use of (11)C-methionine and (18)F-FDG-PET for germinoma in central nervous system. Ann Nucl Med, 2014; 28: 94-102.
- Arima H, Wakabayashi T, Nagatani T, Fujii M, Hirakawa A, Murase T, Yambe Y, Yamada T, Yamakawa F, Yamamori I, Yamauchi M, Oiso Y. Adipsia increases risk of death in patients with central diabetes insipidus. Endocr J, 2014; 61: 143-148.
- Miyachi S, Matsubara N, Izumi T, Asai T, Yamanouchi T, Ota K, Oda K, Wakabayashi T. The 'one and a half round microcatheterization technique' for stent-assisted coil embolization of intracranial aneurysm: technical case series. J Neurointerv Surg, 2014; 6: 357-362.
- 2013
- Matsubara N, Miyachi S, Okamaoto T, Izumi T, Asai T, Yamanouchi T, Ota K, Oda K, Wakabayashi T. Spinal cord infarction is an unusual complication of intracranial neuroendovascular intervention. Interv Neuroradiol, 2013; 19: 500-505.
- Nakahara N, Takebayashi S, Tanei T, Hirano M, Fujii M, Wakabayashi T. [Image-guided surgery for motor eloquent area glioma supported by intraoperative MRI]. No Shinkei Geka, 2013; 41: 1047-1063.
- Wakabayashi T, Natsume A, Fujii M. [Chemotherapy for malignant gliomas: an update]. Gan To Kagaku Ryoho, 2013; 40: 1283-1287.
- Umebayashi D, Hara M, Nakajima Y, Nishimura Y, Wakabayashi T. Posterior fixation for atlantoaxial subluxation in a case with complex anomaly of persistent first intersegmental artery and assimilation in the C1 vertebra. Neurol Med Chir (Tokyo), 2013; 53: 882-886.
- Nishimura Y, Hara M, Natsume A, Nakajima Y, Fukuyama R, Wakabayashi T, Ginsberg HJ. Spinal intradural cystic venous angioma originating from a nerve root in the cauda equina. J Neurosurg Spine, 2013; 19: 716-720.
- Miyachi S, Matsubara N, Izumi T, Asai T, Yamanouchi T, Ota K, Oda K, Wakabayashi T. Stent/balloon combination assist technique for wide-necked basilar terminal aneurysms. Interv Neuroradiol, 2013; 19: 299-305.
- Asai T, Miyachi S, Izumi T, Matsubara N, Yamanouchi T, Ota K, Oda K, Wakabayashi T. [Systematic review of complications for proper informed consent (9) periprocedural complications of carotid artery stenting: a review article]. No Shinkei Geka, 2013; 41: 719-729.
- Tanei T, Kajita Y, Noda H, Takebayashi S, Hirano M, Nakahara N, Wakabayashi T. [Efficacy of tramadol/acetaminophen medication for central post-stroke pain]. No Shinkei Geka, 2013; 41: 679-685.
- Tanei T, Nagatani T, Nakahara N, Watanabe T, Nishihata T, Nielsen ML, Takebayashi S, Hirano M, Wakabayashi T. Use of high-field intraoperative magnetic resonance imaging during endoscopic transsphenoidal surgery for functioning pituitary microadenomas and small adenomas located in the intrasellar region. Neurol Med Chir (Tokyo), 2013; 53: 501-510.
- Nakajima Y, Hara M, Makino K, Umebayashi D, Wakabayashi T. [A case of far lateral lumbar disk herniation treated with Transforaminal Lumbar Interbody Fusion(TLIF)]. No Shinkei Geka, 2013; 41: 629-636.
- Hasegawa H, Hyodo T, Asano E, Ito S, Maeda M, Kuribayashi H, Natsume A, Wakabayashi T, Hamaguchi M, Senga T. The role of PLK1-phosphorylated SVIL in myosin II activation and cytokinetic furrowing. J Cell Sci, 2013; 126: 3627-3637.
- Natsume A, Ito M, Katsushima K, Ohka F, Hatanaka A, Shinjo K, Sato S, Takahashi S, Ishikawa Y, Takeuchi I, Shimogawa H, Uesugi M, Okano H, Kim SU, Wakabayashi T, Issa JP, Sekido Y, Kondo Y. Chromatin regulator PRC2 is a key regulator of epigenetic plasticity in glioblastoma. Cancer Res, 2013; 73: 4559-4570.
- Matsubara N, Miyachi S, Tsukamoto N, Kojima T, Izumi T, Haraguchi K, Asai T, Yamanouchi T, Ota K, Wakabayashi T. Endovascular intervention for acute cervical carotid artery occlusion. Acta Neurochir (Wien), 2013; 155: 1115-1123.
- Fujitani S, Matsuda K, Nakamura F, Baba K, Usui N, Tottori T, Mihara T, Terada K, Usui K, Inoue Y, Kajita Y, Wakabayashi T. Statistical parametric mapping of interictal 123I-iomazenil SPECT in temporal lobe epilepsy surgery. Epilepsy Res, 2013; 106: 173-180.
- Jiang Z, Nimura Y, Hayashi Y, Kitasaka T, Misawa K, Fujiwara M, Kajita Y, Wakabayashi T, Mori K. Anatomical annotation on vascular structure in volume rendered images. Comput Med Imaging Graph, 2013; 37: 131-141.
- Gupta R, Miyachi S, Matsubara N, Izumi T, Naito T, Haraguchi K, Wakabayashi T. A unique type of dural arteriovenous fistula at confluence of sinuses treated with endovascular embolization: a case report. Neurointervention, 2013; 8: 34-40.
- Ando H, Natsume A, Iwami K, Ohka F, Kuchimaru T, Kizaka-Kondoh S, Ito K, Saito K, Sugita S, Hoshino T, Wakabayashi T. A hypoxia-inducible factor (HIF)-3alpha splicing variant, HIF-3alpha4 impairs angiogenesis in hypervascular malignant meningiomas with epigenetically silenced HIF-3alpha4. Biochem Biophys Res Commun, 2013; 433: 139-144.
- Iwami K, Natsume A, Ohno M, Ikeda H, Mineno J, Nukaya I, Okamoto S, Fujiwara H, Yasukawa M, Shiku H, Wakabayashi T. Adoptive transfer of genetically modified Wilms' tumor 1-specific T cells in a novel malignant skull base meningioma model. Neuro Oncol, 2013; 15: 747-758.
- Kajita Y, Yoshida K, Nagai T, Wakabayashi T. [Mood States in outpatients with lesional epilepsy at the neurosurgical clinic and improvement in mood States after lamotrigine addiction]. No Shinkei Geka, 2013; 41: 209-218.
- Nagasaka T, Inao S, Wakabayashi T. What does the CT angiography "spot sign" of intracerebral hemorrhage mean in modern neurosurgical settings with minimally invasive endoscopic techniques? Neurosurg Rev, 2013; 36: 341-348.
- Yamada Y, Nakamura S, Ito K, Umemura E, Hara K, Nagasaka T, Abe A, Baba S, Furuichi Y, Izumi Y, Klein OD, Wakabayashi T. Injectable bone tissue engineering using expanded mesenchymal stem cells. Stem Cells, 2013; 31: 572-580.
- Gupta R, Miyachi S, Matsubara N, Izumi T, Naito T, Haraguchi K, Wakabayashi T. Pial arteriovenous fistula as a cause of bilateral thalamic hyperintensities--an unusual case report and review of the literature. J Neurol Surg A Cent Eur Neurosurg, 2013; 74 Suppl 1: e18-24.
- Nishimura Y, Natsume A, Ito M, Hara M, Motomura K, Fukuyama R, Sumiyoshi N, Aoki I, Saga T, Lee HJ, Wakabayashi T, Kim SU. Interferon-beta delivery via human neural stem cell abates glial scar formation in spinal cord injury. Cell Transplant, 2013; 22: 2187-2201.
- Motomura K, Mittelbronn M, Paulus W, Brokinkel B, Keyvani K, Sure U, Wrede K, Nakazato Y, Tanaka Y, Nonoguchi N, Pierscianek D, Kim YH, Mariani L, Vital A, Perry A, Ohgaki H. PDGFRA gain in low-grade diffuse gliomas. J Neuropathol Exp Neurol, 2013; 72: 61-66.
- Pierscianek D, Kim YH, Motomura K, Mittelbronn M, Paulus W, Brokinkel B, Keyvani K, Wrede K, Nakazato Y, Tanaka Y, Mariani L, Vital A, Sure U, Ohgaki H. MET gain in diffuse astrocytomas is associated with poorer outcome. Brain Pathol, 2013; 23: 13-18.
- 2012
- Nagai T, Kajita Y, Maesawa S, Nakatsubo D, Yoshida K, Kato K, Wakabayashi T. Preoperative regional cerebral blood flow and postoperative clinical improvement in patients with Parkinson's disease undergoing subthalamic nucleus deep brain stimulation. Neurol Med Chir (Tokyo), 2012; 52: 865-872.
- Nishimura Y, Hara M, Natsume A, Takemoto M, Fukuyama R, Wakabayashi T. Intra-extradural dumbbell-shaped hemangioblastoma manifesting as subarachnoid hemorrhage in the cauda equina. Neurol Med Chir (Tokyo), 2012; 52: 659-665.
- Tanei T, Nakahara N, Takebayashi S, Hirano M, Nagatani T, Nishihata T, Wakabayashi T. Endoscopic biopsy for lesions located in the parenchyma of the brain: preoperative planning based on stereotactic methods. Technical note. Neurol Med Chir (Tokyo), 2012; 52: 617-621.
- Tanemura E, Nagatani T, Aimi Y, Kishida Y, Takeuchi K, Wakabayashi T. Quality of life in nonfunctioning pituitary macroadenoma patients before and after surgical treatment. Acta Neurochir (Wien), 2012; 154: 1895-1902.
- Okada Y, Nihashi T, Fujii M, Kato K, Okochi Y, Ando Y, Yamashita M, Maesawa S, Takebayashi S, Wakabayashi T, Naganawa S. Differentiation of newly diagnosed glioblastoma multiforme and intracranial diffuse large B-cell Lymphoma using (11)C-methionine and (18)F-FDG PET. Clin Nucl Med, 2012; 37: 843-849.
- Motomura K, Natsume A, Watanabe R, Ito I, Kato Y, Momota H, Nishikawa R, Mishima K, Nakasu Y, Abe T, Namba H, Nakazato Y, Tashiro H, Takeuchi I, Mori T, Wakabayashi T. Immunohistochemical analysis-based proteomic subclassification of newly diagnosed glioblastomas. Cancer Sci, 2012; 103: 1871-1879.
- Uozumi Y, Sumitomo M, Maruwaka M, Araki Y, Izumi T, Miyachi S, Kato T, Hasegawa T, Kida Y, Okamoto S, Wakabayashi T. Moyamoya syndrome associated with gamma knife surgery for cerebral arteriovenous malformation: case report. Neurol Med Chir (Tokyo), 2012; 52: 343-345.
- Ohno M, Natsume A, Wakabayashi T. Cytokine therapy. Adv Exp Med Biol, 2012; 746: 86-94.
- Haraguchi K, Miyachi S, Izumi T, Matsubara N, Naito T, Asai T, Yamanouchi T, Wakabayashi T. [Resistance to antiplatelet agents assessed by a point-of-care platelet function test and thromboembolic adverse events in neurointervention]. No Shinkei Geka, 2012; 40: 399-406.
- Ohka F, Natsume A, Wakabayashi T. Current trends in targeted therapies for glioblastoma multiforme. Neurol Res Int, 2012; 2012: 878425.
- Tanei T, Nakahara N, Takebayashi S, Hirano M, Wakabayashi T. Simultaneous surgical resections of two distant metastatic malignant melanoma lesions--case report. Nagoya J Med Sci, 2012; 74: 173-179.
- Tanei T, Nakahara N, Takebayashi S, Hirano M, Kajita Y, Wakabayashi T. [Dual lead spinal cord stimulation using octad lead for central post-stroke pain]. No Shinkei Geka, 2012; 40: 325-329.
- Iwami K, Shimato S, Ohno M, Okada H, Nakahara N, Sato Y, Yoshida J, Suzuki S, Nishikawa H, Shiku H, Natsume A, Wakabayashi T. Peptide-pulsed dendritic cell vaccination targeting interleukin-13 receptor alpha2 chain in recurrent malignant glioma patients with HLA-A*24/A*02 allele. Cytotherapy, 2012; 14: 733-742.
- Naito T, Miyachi S, Matsubara N, Isoda H, Izumi T, Haraguchi K, Takahashi I, Ishii K, Wakabayashi T. Magnetic resonance fluid dynamics for intracranial aneurysms--comparison with computed fluid dynamics. Acta Neurochir (Wien), 2012; 154: 993-1001.
- Kishida Y, Natsume A, Toda H, Toi Y, Motomura K, Koyama H, Matsuda K, Nakayama O, Sato M, Suzuki M, Kondo Y, Wakabayashi T. Correlation between quantified promoter methylation and enzymatic activity of O6-methylguanine-DNA methyltransferase in glioblastomas. Tumour Biol, 2012; 33: 373-381.
- Iwami K, Momota H, Natsume A, Kinjo S, Nagatani T, Wakabayashi T. A novel method of intracranial injection via the postglenoid foramen for brain tumor mouse models. J Neurosurg, 2012; 116: 630-635.
- Kishida Y, Natsume A, Kondo Y, Takeuchi I, An B, Okamoto Y, Shinjo K, Saito K, Ando H, Ohka F, Sekido Y, Wakabayashi T. Epigenetic subclassification of meningiomas based on genome-wide DNA methylation analyses. Carcinogenesis, 2012; 33: 436-441.
- Motomura K, Mittelbronn M, Paulus W, Brokinkel B, Keyvani K, Sure U, Wrede K, Nakazato Y, Tanaka Y, Pierscianek D, Kim YH, Mariani L, Vital A, Ohgaki H. DMBT1 homozygous deletion in diffuse astrocytomas is associated with unfavorable clinical outcome. J Neuropathol Exp Neurol, 2012; 71: 702-707.
- 2011
- Wakabayashi T. [Clinical trial updates for malignant brain tumors]. Rinsho Shinkeigaku, 2011; 51: 853-856.
- Hayashi S, Osuka K, Watanabe Y, Yasuda M, Takayasu M, Wakabayashi T. Hypothermia enhances the colocalization of calmodulin kinase IIalpha with neuronal nitric oxide synthase in the hippocampus following cerebral ischemia. Neurosci Lett, 2011; 505: 228-232.
- Ohka F, Natsume A, Motomura K, Kishida Y, Kondo Y, Abe T, Nakasu Y, Namba H, Wakai K, Fukui T, Momota H, Iwami K, Kinjo S, Ito M, Fujii M, Wakabayashi T. The global DNA methylation surrogate LINE-1 methylation is correlated with MGMT promoter methylation and is a better prognostic factor for glioma. PLoS One, 2011; 6: e23332.
- Motomura K, Natsume A, Fujii M, Ito M, Momota H, Wakabayashi T. Long-term survival in patients with newly diagnosed primary central nervous system lymphoma treated with dexamethasone, etoposide, ifosfamide and carboplatin chemotherapy and whole-brain radiation therapy. Leuk Lymphoma, 2011; 52: 2069-2075.
- Iwami K, Natsume A, Wakabayashi T. Cytokine networks in glioma. Neurosurg Rev, 2011; 34: 253-263; discussion 263-254.
- Fujii M, Miyachi S, Matsubara N, Kinkori T, Takebayashi S, Izumi T, Ohshima T, Tsurumi A, Hososhima O, Wakabayashi T, Yoshida J. Selective propofol injection into the M1 segment of the middle cerebral artery (MCA Wada test) reduces adverse effects and enhances the reliability of the Wada test for determining speech dominance. World Neurosurg, 2011; 75: 503-508.
- Ichikawa T, Miyachi S, Izumi T, Matsubara N, Naito T, Haraguchi K, Wakabayashi T, Koketsu N. Fenestration of a supraclinoid internal carotid artery associated with dual aneurysms: case report. Neurosurgery, 2011; 69: E1005-1008; discussion E1009.
- Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Inao S, Wakabayashi T. A novel monoshaft bipolar cautery for use in endoscopic intracranial surgery. A short technical note. Clin Neurol Neurosurg, 2011; 113: 607-611.
- Motomura K, Natsume A, Kishida Y, Higashi H, Kondo Y, Nakasu Y, Abe T, Namba H, Wakai K, Wakabayashi T. Benefits of interferon-beta and temozolomide combination therapy for newly diagnosed primary glioblastoma with the unmethylated MGMT promoter: A multicenter study. Cancer, 2011; 117: 1721-1730.
- Wakabayashi T, Kayama T, Nishikawa R, Takahashi H, Hashimoto N, Takahashi J, Aoki T, Sugiyama K, Ogura M, Natsume A, Yoshida J. A multicenter phase I trial of combination therapy with interferon-beta and temozolomide for high-grade gliomas (INTEGRA study): the final report. J Neurooncol, 2011; 104: 573-577.
- Natsume A, Kinjo S, Yuki K, Kato T, Ohno M, Motomura K, Iwami K, Wakabayashi T. Glioma-initiating cells and molecular pathology: implications for therapy. Brain Tumor Pathol, 2011; 28: 1-12.
- Tanei T, Nakahara N, Takebayashi S, Ito M, Hashizume Y, Wakabayashi T. Primary angiitis of the central nervous system mimicking tumor-like lesion--case report. Neurol Med Chir (Tokyo), 2011; 51: 56-59.
- Tanei T, Kajita Y, Noda H, Takebayashi S, Nakatsubo D, Maesawa S, Wakabayashi T. Efficacy of motor cortex stimulation for intractable central neuropathic pain: comparison of stimulation parameters between post-stroke pain and other central pain. Neurol Med Chir (Tokyo), 2011; 51: 8-14.
- Momota H, Iwami K, Fujii M, Motomura K, Natsume A, Ogino J, Hasegawa T, Wakabayashi T. Rhabdoid glioblastoma in a child: case report and literature review. Brain Tumor Pathol, 2011; 28: 65-70.
- Matsubara N, Miyachi S, Tsukamoto N, Izumi T, Naito T, Haraguchi K, Wakabayashi T. Endovascular coil embolization for saccular-shaped blood blister-like aneurysms of the internal carotid artery. Acta Neurochir (Wien), 2011; 153: 287-294.
- Mitsui T, Fujii M, Tsuzaka M, Hayashi Y, Asahina Y, Wakabayashi T. Skin shift and its effect on navigation accuracy in image-guided neurosurgery. Radiol Phys Technol, 2011; 4: 37-42.
- Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Inao S, Wakabayashi T. Early recovery and better evacuation rate in neuroendoscopic surgery for spontaneous intracerebral hemorrhage using a multifunctional cannula: preliminary study in comparison with craniotomy. J Stroke Cerebrovasc Dis, 2011; 20: 208-213.
- Matsubara N, Miyachi S, Nagano Y, Ohshima T, Hososhima O, Izumi T, Tsurumi A, Wakabayashi T, Sano A, Fujimoto H. Evaluation of the characteristics of various types of coils for the embolization of intracranial aneurysms with an optical pressure sensor system. Neuroradiology, 2011; 53: 169-175.
- 2010
- Maesawa S, Fujii M, Nakahara N, Watanabe T, Wakabayashi T, Yoshida J. Intraoperative tractography and motor evoked potential (MEP) monitoring in surgery for gliomas around the corticospinal tract. World Neurosurg, 2010; 74: 153-161.
- Araki Y, Yoshikawa K, Okamoto S, Sumitomo M, Maruwaka M, Wakabayashi T. Identification of novel biomarker candidates by proteomic analysis of cerebrospinal fluid from patients with moyamoya disease using SELDI-TOF-MS. BMC Neurol, 2010; 10: 112.
- Mizuno M, Wakabayashi T. [Brain tumor]. Nihon Rinsho, 2010; 68 Suppl 8: 623-626.
- Natsume A, Motomura K, Wakabayashi T. [The genome atlas of brain tumors]. Nihon Rinsho, 2010; 68 Suppl 8: 473-480.
- Iwami K, Natsume A, Wakabayashi T. Gene therapy for high-grade glioma. Neurol Med Chir (Tokyo), 2010; 50: 727-736.
- Ohno M, Natsume A, Ichiro Iwami K, Iwamizu H, Noritake K, Ito D, Toi Y, Ito M, Motomura K, Yoshida J, Yoshikawa K, Wakabayashi T. Retrovirally engineered T-cell-based immunotherapy targeting type III variant epidermal growth factor receptor, a glioma-associated antigen. Cancer Sci, 2010; 101: 2518-2524.
- Ito E, Saito K, Nagatani T, Ishiyama J, Terada K, Yoshida M, Wakabayashi T. Intradural cranial chordoma. World Neurosurg, 2010; 73: 194-197; discussion e131.
- Motomura K, Ogura M, Natsume A, Yokoyama H, Wakabayashi T. A free-radical scavenger protects the neural progenitor cells in the dentate subgranular zone of the hippocampus from cell death after X-irradiation. Neurosci Lett, 2010; 485: 65-70.
- Tanei T, Takebayashi S, Nishihata T, Nakahara N, Wakabayashi T. [Removal of an arteriovenous malformation near the pyramidal tract using the neuronavigation system: a case report]. No Shinkei Geka, 2010; 38: 745-750.
- Tanei T, Kajita Y, Wakabayashi T. Motor cortex stimulation for intractable neuropathic facial pain related to multiple sclerosis. Neurol Med Chir (Tokyo), 2010; 50: 604-607.
- Natsume A, Kondo Y, Ito M, Motomura K, Wakabayashi T, Yoshida J. Epigenetic aberrations and therapeutic implications in gliomas. Cancer Sci, 2010; 101: 1331-1336.
- Tanaka Y, Yu Q, Doumoto K, Sano A, Hayashi Y, Fujii M, Kajita Y, Mizuno M, Wakabayashi T, Fujimoto H. Development of a real-time tactile sensing system for brain tumor diagnosis. Int J Comput Assist Radiol Surg, 2010; 5: 359-367.
- Watanabe Y, Hayashi Y, Fujii M, Kimura M, Sugiura A, Tsuzaka M, Wakabayashi T. [Development of automatic navigation measuring system using template-matching software in image guided neurosurgery]. Nihon Hoshasen Gijutsu Gakkai Zasshi, 2010; 66: 131-136.
- Nakajima Y, Osuka K, Seki Y, Gupta RC, Hara M, Takayasu M, Wakabayashi T. Taurine reduces inflammatory responses after spinal cord injury. J Neurotrauma, 2010; 27: 403-410.
- 2009
- Wakabayashi T, Fujii M, Kajita Y, Natsume A, Maezawa S, Yoshida J. Advanced new neurosurgical procedure using integrated system of intraoperative MRI and neuronavigation with multimodal neuroradiological images. Nagoya J Med Sci, 2009; 71: 101-107.
- Tanei T, Kajita Y, Nihashi T, Kaneoke Y, Takebayashi S, Nakatsubo D, Wakabayashi T. Changes in regional blood flow induced by unilateral subthalamic nucleus stimulation in patients with Parkinson's disease. Neurol Med Chir (Tokyo), 2009; 49: 507-513.
- Ohno M, Natsume A, Kondo Y, Iwamizu H, Motomura K, Toda H, Ito M, Kato T, Wakabayashi T. The modulation of microRNAs by type I IFN through the activation of signal transducers and activators of transcription 3 in human glioma. Mol Cancer Res, 2009; 7: 2022-2030.
- Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Takagawa Y, Inao S, Wakabayashi T. Balanced irrigation-suction technique with a multifunctional suction cannula and its application for intraoperative hemorrhage in endoscopic evacuation of intracerebral hematomas: technical note. Neurosurgery, 2009; 65: E826-827; discussion E827.
- Ito E, Saito K, Nagatani T, Teranishi M, Aimi Y, Wakabayashi T. Cavernous sinus thrombophlebitis caused by porphyromonas gingivalis with abscess formation extending to the orbital cavity. Case report. Neurol Med Chir (Tokyo), 2009; 49: 370-373.
- Maesawa S, Fujii M, Nakahara N, Watanabe T, Saito K, Kajita Y, Nagatani T, Wakabayashi T, Yoshida J. Clinical indications for high-field 1.5 T intraoperative magnetic resonance imaging and neuro-navigation for neurosurgical procedures. Review of initial 100 cases. Neurol Med Chir (Tokyo), 2009; 49: 340-349; discussion 349-350.
- Fujii M, Wakabayashi T. [Image-guided neurosurgery using intraoperative MRI]. Brain Nerve, 2009; 61: 823-834.
- Natsume A, Kondo Y, Wakabayashi T. [Epigenetic analyses of brain tumor stem cells]. Brain Nerve, 2009; 61: 791-798.
- Watanabe Y, Fujii M, Hayashi Y, Kimura M, Murai Y, Hata M, Sugiura A, Tsuzaka M, Wakabayashi T. Evaluation of errors influencing accuracy in image-guided neurosurgery. Radiol Phys Technol, 2009; 2: 120-125.
- Yuki K, Natsume A, Yokoyama H, Kondo Y, Ohno M, Kato T, Chansakul P, Ito M, Kim SU, Wakabayashi T. Induction of oligodendrogenesis in glioblastoma-initiating cells by IFN-mediated activation of STAT3 signaling. Cancer Lett, 2009; 284: 71-79.
- Tanei T, Kajita Y, Kaneoke Y, Takebayashi S, Nakatsubo D, Wakabayashi T. Staged bilateral deep brain stimulation of the subthalamic nucleus for the treatment of Parkinson's disease. Acta Neurochir (Wien), 2009; 151: 589-594.
- Ohno M, Natsume A, Fujii M, Ito M, Wakabayashi T. Interferon-beta, MCNU, and conventional radiotherapy for pediatric patients with brainstem glioma. Pediatr Blood Cancer, 2009; 53: 37-41.
- Matsubara N, Miyachi S, Nagano Y, Ohshima T, Hososhima O, Izumi T, Tsurumi A, Wakabayashi T, Sakaguchi M, Sano A, Fujimoto H. A novel pressure sensor with an optical system for coil embolization of intracranial aneurysms. Laboratory investigation. J Neurosurg, 2009; 111: 41-47.
- Wakabayashi T, Natsume A, Hatano H, Fujii M, Shimato S, Ito M, Ohno M, Ito S, Ogura M, Yoshida J. p16 promoter methylation in the serum as a basis for the molecular diagnosis of gliomas. Neurosurgery, 2009; 64: 455-461; discussion 461-452.
- Ito M, Natsume A, Takeuchi H, Shimato S, Ohno M, Wakabayashi T, Yoshida J. Type I interferon inhibits astrocytic gliosis and promotes functional recovery after spinal cord injury by deactivation of the MEK/ERK pathway. J Neurotrauma, 2009; 26: 41-53.
- Kurimoto F, Saito K, Watanabe T, Nagatani T, Nishiwaki K, Wakabayashi T, Iwase S. Preliminary measurement of intraoperative sympathetic nerve activity using microneurography and laser Doppler flowmetry during surgical resection of suprasellar tumors. Neurol Med Chir (Tokyo), 2009; 49: 13-21.
- Oi S, Natsume A, Ito M, Kondo Y, Shimato S, Maeda Y, Saito K, Wakabayashi T. Synergistic induction of NY-ESO-1 antigen expression by a novel histone deacetylase inhibitor, valproic acid, with 5-aza-2'-deoxycytidine in glioma cells. J Neurooncol, 2009; 92: 15-22.
- 2008
- Wakabayashi T, Kayama T, Nishikawa R, Takahashi H, Yoshimine T, Hashimoto N, Aoki T, Kurisu K, Natsume A, Ogura M, Yoshida J. A multicenter phase I trial of interferon-beta and temozolomide combination therapy for high-grade gliomas (INTEGRA Study). Jpn J Clin Oncol, 2008; 38: 715-718.
- Shimato S, Natsume A, Wakabayashi T, Tsujimura K, Nakahara N, Ishii J, Ito M, Akatsuka Y, Kuzushima K, Yoshida J. Identification of a human leukocyte antigen-A24-restricted T-cell epitope derived from interleukin-13 receptor alpha2 chain, a glioma-associated antigen. J Neurosurg, 2008; 109: 117-122.
- Natsume A, Wakabayashi T, Tsujimura K, Shimato S, Ito M, Kuzushima K, Kondo Y, Sekido Y, Kawatsura H, Narita Y, Yoshida J. The DNA demethylating agent 5-aza-2'-deoxycytidine activates NY-ESO-1 antigenicity in orthotopic human glioma. Int J Cancer, 2008; 122: 2542-2553.
- Wakabayashi T. [Treatment of marignant brain tumor: today and tomorrow]. No Shinkei Geka, 2008; 36: 81-82.
- Wakabayashi T, Natsume A, Hashizume Y, Fujii M, Mizuno M, Yoshida J. A phase I clinical trial of interferon-beta gene therapy for high-grade glioma: novel findings from gene expression profiling and autopsy. J Gene Med, 2008; 10: 329-339.
- Natsume A, Wakabayashi T, Ishii D, Maruta H, Fujii M, Shimato S, Ito M, Yoshida J. A combination of IFN-beta and temozolomide in human glioma xenograft models: implication of p53-mediated MGMT downregulation. Cancer Chemother Pharmacol, 2008; 61: 653-659.
- 2007
- Takeuchi H, Natsume A, Wakabayashi T, Aoshima C, Shimato S, Ito M, Ishii J, Maeda Y, Hara M, Kim SU, Yoshida J. Intravenously transplanted human neural stem cells migrate to the injured spinal cord in adult mice in an SDF-1- and HGF-dependent manner. Neurosci Lett, 2007; 426: 69-74.
- Ishii D, Natsume A, Wakabayashi T, Hatano H, Asano Y, Takeuchi H, Shimato S, Ito M, Fujii M, Yoshida J. Efficacy of temozolomide is correlated with 1p loss and methylation of the deoxyribonucleic acid repair gene MGMT in malignant gliomas. Neurol Med Chir (Tokyo), 2007; 47: 341-349; discussion 350.
- Nakane Y, Natsume A, Wakabayashi T, Oi S, Ito M, Inao S, Saito K, Yoshida J. Malignant transformation-related genes in meningiomas: allelic loss on 1p36 and methylation status of p73 and RASSF1A. J Neurosurg, 2007; 107: 398-404.
- Ito M, Wakabayashi T, Natsume A, Hatano H, Fujii M, Yoshida J. Genetically heterogeneous glioblastoma recurring with disappearance of 1p/19q losses: case report. Neurosurgery, 2007; 61: E168-169; discussion E169.
- Tsuno T, Natsume A, Katsumata S, Mizuno M, Fujita M, Osawa H, Nakahara N, Wakabayashi T, Satoh Y, Inagaki M, Yoshida J. Inhibition of Aurora-B function increases formation of multinucleated cells in p53 gene deficient cells and enhances anti-tumor effect of temozolomide in human glioma cells. J Neurooncol, 2007; 83: 249-258.
- 2006
- Wakabayashi T, Natsume A, Yoshida J. [Glioma]. Nihon Rinsho, 2006; 64: 1327-1332.
- Hatano H, Wakabayashi T, Yoshida J. [Pineal lesion tumors (germinoma)]. Nihon Rinsho, 2006; Suppl 1: 178-182.
- Shimato S, Mitsudomi T, Kosaka T, Yatabe Y, Wakabayashi T, Mizuno M, Nakahara N, Hatano H, Natsume A, Ishii D, Yoshida J. EGFR mutations in patients with brain metastases from lung cancer: association with the efficacy of gefitinib. Neuro Oncol, 2006; 8: 137-144.
- Shimato S, Wakabayashi T, Mizuno M, Nakahara N, Hatano H, Natsume A, Ishii D, Hasegawa Y, Hyodo I, Nagasaka T, Yoshida J. Brain metastases from apocrine carcinoma of the scalp: case report. J Neurooncol, 2006; 77: 285-289.
- 2005
- Wakabayashi T, Saito K, Yoshida J. [Neurofibromatosis ]. Nihon Rinsho, 2005; 63 Suppl 9: 164-169.
- Natsume A, Ishii D, Wakabayashi T, Tsuno T, Hatano H, Mizuno M, Yoshida J. IFN-beta down-regulates the expression of DNA repair gene MGMT and sensitizes resistant glioma cells to temozolomide. Cancer Res, 2005; 65: 7573-7579.
- Arima T, Natsume A, Hatano H, Nakahara N, Fujita M, Ishii D, Wakabayashi T, Doyu M, Nagasaka T, Yoshida J. Intraventricular chordoid meningioma presenting with Castleman disease due to overproduction of interleukin-6. Case report. J Neurosurg, 2005; 102: 733-737.
- 2004
- Fujita M, Mizuno M, Nagasaka T, Wakabayashi T, Maeda K, Ishii D, Arima T, Kawajiri A, Inagaki M, Yoshida J. Aurora-B dysfunction of multinucleated giant cells in glioma detected by site-specific phosphorylated antibodies. J Neurosurg, 2004; 101: 1012-1017.
- Yoshida J, Mizuno M, Wakabayashi T. Interferon-beta gene therapy for cancer: basic research to clinical application. Cancer Sci, 2004; 95: 858-865.
- Yoshida J, Mizuno M, Fujii M, Kajita Y, Nakahara N, Hatano M, Saito R, Nobayashi M, Wakabayashi T. Human gene therapy for malignant gliomas (glioblastoma multiforme and anaplastic astrocytoma) by in vivo transduction with human interferon beta gene using cationic liposomes. Hum Gene Ther, 2004; 15: 77-86.
- 2003
- Takasu S, Takahashi T, Okamoto S, Oriuchi N, Nakayashiki N, Okamoto K, Muramatsu H, Hayashi T, Nakahara N, Mizuno M, Wakabayashi T, Higuchi T, Endo K, Kozaki K, Miyaishi O, Saga S, Ueda R, Yoshida J, Yoshikawa K. Radioimmunoscintigraphy of intracranial glioma xenograft with a technetium-99m-labeled mouse monoclonal antibody specifically recognizing type III mutant epidermal growth factor receptor. J Neurooncol, 2003; 63: 247-256.
- Nakahara N, Pollack IF, Storkus WJ, Wakabayashi T, Yoshida J, Okada H. Effective induction of antiglioma cytotoxic T cells by coadministration of interferon-beta gene vector and dendritic cells. Cancer Gene Ther, 2003; 10: 549-558.
- Maeda K, Mizuno M, Wakabayashi T, Takasu S, Nagasaka T, Inagaki M, Yoshida J. Morphological assessment of the development of multinucleated giant cells in glioma by using mitosis-specific phosphorylated antibodies. J Neurosurg, 2003; 98: 854-859.
- Ito A, Shinkai M, Honda H, Yoshikawa K, Saga S, Wakabayashi T, Yoshida J, Kobayashi T. Heat shock protein 70 expression induces antitumor immunity during intracellular hyperthermia using magnetite nanoparticles. Cancer Immunol Immunother, 2003; 52: 80-88.
- 2002
- Ohno T, Wakabayashi T, Takemura A, Yoshida J, Ito A, Shinkai M, Honda H, Kobayashi T. Effective solitary hyperthermia treatment of malignant glioma using stick type CMC-magnetite. In vivo study. J Neurooncol, 2002; 56: 233-239.
Research Keywords
Lower grade gliomas, Grade II and III gliomas, next-generation sequencer, Chimeric antigen receptor, CAR T cell therapy , Podoplanin , IDH1 mutation, immuno-wall microdevice, TMS, awake brain mapping, awake surgery, moyamoya disease, nitric oxide synthase, endoscope, minimally invasive neurosurgery, device development, hydrocephalus, ciliary dyskinesia, dynein, EEG-fMRI, stereotactic robotic device, MRgFUS: MRI guided fucused ultrasound treatment, Epilepsy, Parkinson disease, Essesntial tremor, medulloblastoma, Acquired Chiari type 1 like malformation, dural arteriovenous fistula, Computational fluid dynamics, medical-engineering collaboration